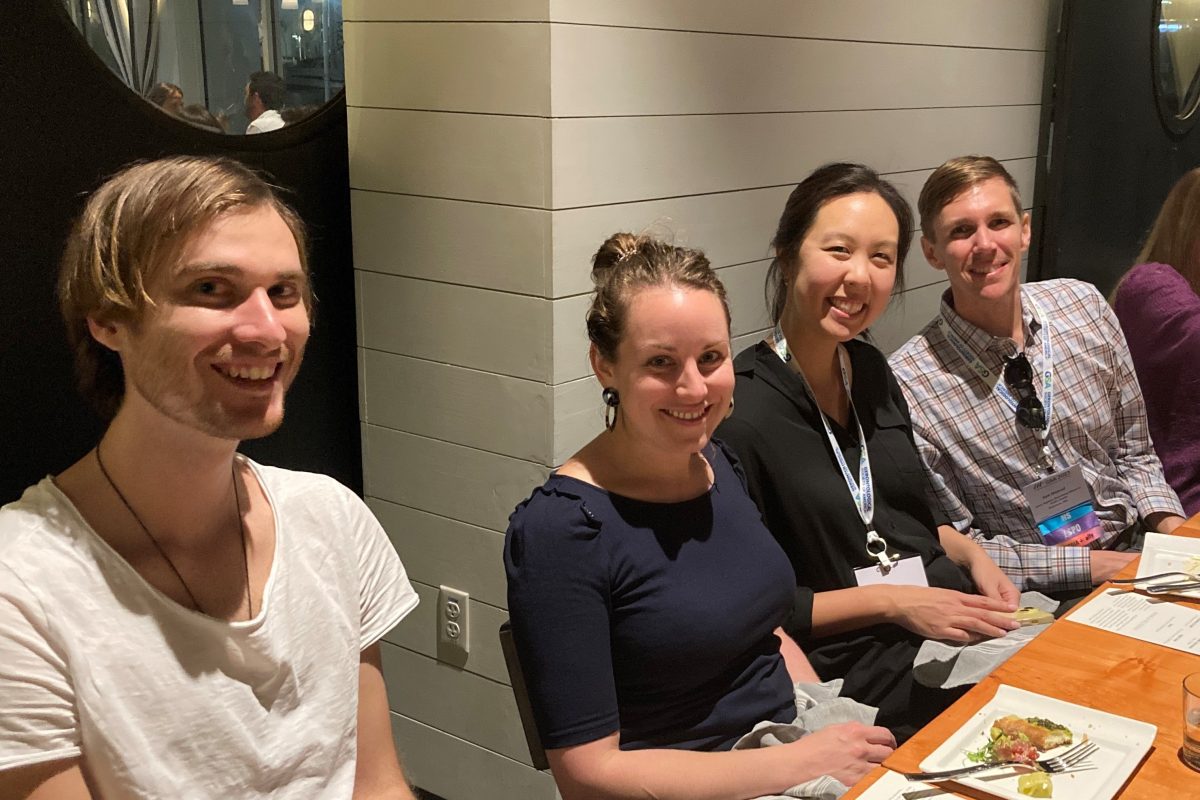
Johns Hopkins University (JHU) and the Center on Aging and Health (COAH) were well-represented at this year’s Annual Meeting of the Gerontological Society of America (GSA) in Tampa, Florida. Faculty, fellows, and students from the Center, as well as many COAH alumni, led symposia talks, engaged in special sessions, and presented posters during this 5-day meeting. COAH hosted a dinner to reunite past and present team members and to celebrate the Center’s collective successes and future collaborations in aging research. Please see the photo gallery!
It is that time of year when families start to gather over seasonal harvest celebrations and give thanks, and our hearts open with gratitude. In addition to Thanksgiving, November is also National Family Caregiver’s Month, which underscores the appreciation our society has for those who tend to loved ones in need of support. With this sense of appreciation, celebration, and recognition, we are delighted to announce that Dr. Kimberly Skarupski is our Fall 2023 COAH Champion. Dr. Skarupski serves the Johns Hopkins University School of Medicine community as Senior Associate Dean for Faculty Development. She is Senior Associate Faculty with COAH, and she holds joint professor appointments in the Division of Geriatric Medicine and Gerontology in the School of Medicine, as well as with the Department of Epidemiology in the Bloomberg School of Public Health. Also, she is a Certified Professional Coach with the College of Executive Coaching. She is well-known at Johns Hopkins for her research about our own faculty who are also caregivers—and the implications and impact caregiving has on academic careers and the future of medicine.
In fact, in March 2023, Dr. Skarupski delivered an outstanding, interactive workshop-style COAH Scientific Seminar: “Who Cares? Family Caregiving Experiences of our Healthcare Providers,” where she discussed the findings from a caregiving survey conducted with the faculty of the Department of Medicine in October 2022 based on research she led and conducted with COAH colleagues Drs. David L. Roth (Geriatric Medicine & Gerontology) and Chris Durso (Executive Vice Chair for the Department of Medicine, Johns Hopkins University, and Director of the Department of Medicine for the Johns Hopkins Bayview Medical Center). Together they published an article about it in 2021 entitled, “Prevalence of caregiving and high caregiving strain among late-career medical school faculty members: Workforce, policy and faculty development implications.” For those who missed it, Dr. Skarupski’s seminar was recorded, and you can view it at: “Who Cares? Family Caregiving Experiences of our Healthcare Providers.” Additionally, she prepared a worksheet for seminar participants to use; if you would like to review the insightful content at your own pace, here is the PowerPoint . The top take-aways from Dr. Skarupski’s presentation are:
- The average age of faculty in the Hopkins SOM is 51.7; 28% are age 55+ (2021 data).
- Increased life expectancy + no mandatory retirement age + estimated physician shortage + lower fertility rates = an older faculty population with increasing caregiving responsibilities and needs!
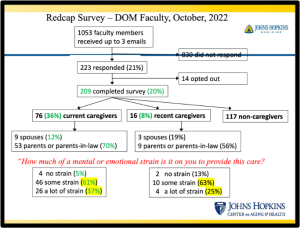
- More than half (58%) of DOM faculty survey respondents (N=209) reported current, recent, or a desire to be (if they had enough time) caregivers; 36% are currently providing care.
- Most current caregivers are women (63%), but 30% of men are current caregivers (gender differences in caregiving are diminishing)!
- 94% report that their caregiving is associated with some or a lot of strain.
- Hopkins’ resources: Only one-third of respondents were aware of “Backup care” and MySupport”; 13% were aware of Hopkins-assisted referrals and 8% of Lifemart. 73% know about the dependent care Flexible Spending accounts. Ratings of Hopkins’ resources ranged from 2.0-3.9 (where 1 is very dissatisfied and 5 is very satisfied). Ratings of other external resources ranged from 3.8-5.0 (see 2 slides below).
- Specific challenges: (a) when parents are out-of-state/out-of-country; (b) sandwich generation (tweeners) caring for older loved ones and children/grandchildren; (c) having to choose between career and caregiving.
- Respondents and seminar participant recommendations: (a) better quality resources; (b) resource/benefit concierge/liaison; (c) curated/vetted lists of resources, by area and state; (d) map to navigate hospital via wheelchair/assisted devices; (e) reduce administrative/EHR/research burdens; (f) provide emotional/social support infrastructure; and (g) the perennial call to make Hopkins’ salaries competitive-enough for faculty to come and stay.
We are pleased to bring you this interview with Dr. Kimberly Skarupski to get to know her better as an amazing person and an exemplary professional.
Tony Teano: Thank you for making time for this interview. Let’s begin with your background, education, and path to COAH.
Dr. Skarupski: I started my education in the Erie, Pennsylvania, public library and subsequently replicated the library in my childhood playroom. My three younger siblings did not appreciate my Dewey-Decimal-system-ing all our books, nor did they appreciate my: book check-out system including date stamp; late-fees; or required book reports. They did, however, appreciate the fact that they all started kindergarten knowing the alphabet, their numbers, and how to spell my name (not theirs).
I’m a liberal arts lover and finally landed on sociology in my undergraduate training at Gannon University in my hometown. I continued for my MA in sociology at SUNY Buffalo, then a PhD in sociology at Case Western Reserve University in Cleveland. It was at Case where I was able to focus on gerontology and epidemiology. I did my post-doctoral fellowship at the University of Michigan at the Institute of Gerontology. And a few years later, I earned my MPH at the University of Pittsburgh, where I focused on epidemiology, program evaluation, and ethnic minority aging.
My first academic appointment was at Bowling Green State University in the department of gerontology. After stints at the University of Arizona and Penn State, I was doing my best gerontologic research at Rush University Medical Center at the Rush Institute for Healthy Aging. After 10 years there, I was fortunate to move to Hopkins as the Assistant Dean for Faculty Development, and also to be welcomed into the COAH family.
Tony Teano: Tell us about your job.
Dr. Skarupski: After 10.5 years at Hopkins, I’m the Senior Associate Dean for Faculty Development, where I get to help faculty members in the School of Medicine along the entire career spectrum. In the Office of Faculty Development, we run new faculty orientation, provide numerous career and professional development seminars, workshops, and leadership programs, offer mentoring and coaching, promotion sessions, late-career and retirement planning, and much more.
Tony Teano: What programming does your office have lined up for faculty over the next few months?
Dr. Skarupski: We always have awesome and interactive sessions: promotions; scholarly writing; grant-writing; lots of education gems – on teaching, curriculum development, scholarship; leadership programs, etc. (If you’re a faculty member in the SOM, search your TRASH for our monthly email!)
Tony Teano: Without question, you are a fabulous leader. What is your leadership style?
Dr. Skarupski: I was asked that question recently and didn’t really know how to answer. My mental rolodex immediately spit-out into my thought bubble things like, “the kind of a leader who is the first-born, Aquarius, ENTJ, Clifton Strengths: input; strategic; futuristic; achiever; intellectual; curious; and non-judgmental Christian. So, while I aim to be humble and wise, I sometimes act-up like a first-born, bossy pants. But that’s a lot. Let’s just say that my life-long career mission/mantra is “to build community.” I am committed to always putting our faculty first AND being a good servant-leader.
Tony Teano: What is the best part of your job?
Dr. Skarupski: The best part of my job is sharing time and space with faculty members. I love to help faculty members by providing resources and information, facilitating connections, and building community.
Tony Teano: What is your best piece of advice about career development?
Dr. Skarupski: “Knowing yourself is the beginning of all wisdom,” by Aristotle. Take some time to know yourself so you can better manage yourself, and then manage and lead others. Start with your values. Align your choices, behaviors, and time with your values.
Tony Teano: That is truly awesome advice. On a tangentially related topic, I know you are a certified professional coach. What do you like best about being a coach?
Dr. Skarupski: I adore coaching. First of all, as an off-the-chart extrovert, I love meeting people. Second, I am super curious—which is a must for a coach. Third, I am NOT non-judgmental—which is another must for a coach—so coaching makes me practice being non-judgmental, and it also makes me practice what my “WAIT” sticky-note reminds me: “why am I talking?” What I love best is helping faculty members—seeing, hearing, feeling, and knowing that I’m making a positive difference.
Tony Teano: November is National Caregiver’s Month, and you are an expert in family caregiving research particularly as the subject pertains to faculty needs at JHU. What is your #1 piece of advice for caregivers?
Dr. Skarupski: Take breaks—get respite care.
Tony Teano: Tell us about your academic research in geriatrics and epidemiology, and what drives your curiosity in these fields.
Dr. Skarupski: I suffer from the malady that befalls many academics–an untethered curiosity that sometimes results in a scolding of “being a mile wide and an inch-deep.” I often say that my brain is a zombie in that my brain craves other brains. I go where my curiosity leads me, which is to other smart people, interesting questions, and ideas.
Historically, you’ll see that my scholarship employed a large-scale epidemiologic database and methodologic approach applied over a variety of settings and topics among older adults, such as nursing homes, neighborhoods, adult day care, prison, dietary patterns, depression, disability, religiosity, etc. Over the past almost decade, I’ve been able to marry my love of all things gerontology with faculty development; specifically in my research exploring factors associated with retirement decisions, institutional policies and priorities around faculty retirement, later-career programs, and faculty caregiving trends and needs.
Tony Teano: Why did you decide to focus on these areas of research? 
Dr. Skarupski: I didn’t learn the term “gerontology” until I took a class in my undergraduate training. I was then very fortunate to have access to an excellent gerontology program in my PhD training at Case Western Reserve, led by Dr. Eva Kahana. My family will tell you that I was born an “old-lady” and always sought-out the company of the most senior and the wisest people at a party… that might explain my proclivity toward Bingo!
Tony Teano: A few years ago, you wrote a book titled, WAG Your Work. I know that WAG is an acronym for “Writing Accountability Groups.” What is this about, and who should read it?
Dr. Skarupski: It’s a brain-dump of the more than 200 times I have given the “WAG talk.” I literally recorded 3 of those presentations, downloaded the recordings and tried to capture the encouragement into book format. It’s meant to be a workbook to inspire faculty members to make writing a sustainable habit using a WAG as a tool.
Tony Teano: You are the host of the “Faculty Factory” podcast. What does the podcast seek to do? What is the latest episode about?
 Dr. Skarupski: We started The Faculty Factory international community almost 5 years ago now and episodes drop every Friday. It is intended to share tools to build leaders. As of November 1, 2023, the Faculty Factory podcast has had 81,626 total downloads, the Faculty Factory YouTube channel has listeners in 94 countries, and the Faculty Factory website has drawn 39,659 web visits from users in 122 countries. Related to the podcast, the free eBook, Habits and Hacks from Hopkins (H3) (published in June, 2022) has been downloaded 401 times, and the first free eBook published in the summer of 2021, Snippets for Success: An eBook Brought to You by the Faculty Factory Community, has been downloaded 1,153 times. You can also follow us on Twitter https://twitter.com/Faculty_Factory.
Dr. Skarupski: We started The Faculty Factory international community almost 5 years ago now and episodes drop every Friday. It is intended to share tools to build leaders. As of November 1, 2023, the Faculty Factory podcast has had 81,626 total downloads, the Faculty Factory YouTube channel has listeners in 94 countries, and the Faculty Factory website has drawn 39,659 web visits from users in 122 countries. Related to the podcast, the free eBook, Habits and Hacks from Hopkins (H3) (published in June, 2022) has been downloaded 401 times, and the first free eBook published in the summer of 2021, Snippets for Success: An eBook Brought to You by the Faculty Factory Community, has been downloaded 1,153 times. You can also follow us on Twitter https://twitter.com/Faculty_Factory.
Tony Teano: What are you currently researching?
Dr. Skarupski: I’m preparing for another national survey on late-career faculty members sponsored by the AAMC!
 Tony Teano: That will be amazing! Now, let’s get to know more about you as a person outside of Johns Hopkins…. I know you have an animal companion at home. Tell us about your furry four-legged friend!
Tony Teano: That will be amazing! Now, let’s get to know more about you as a person outside of Johns Hopkins…. I know you have an animal companion at home. Tell us about your furry four-legged friend!
Dr. Skarupski: I rescued my now 6-year-old Golden Doodle off of petfinder.com right after COVID. His name was and is “Sunny,” which was also my nickname growing up… There’s no such thing as coincidences. Meant to be!
Tony Teano: Where do you like to go on a day trip to unwind and get away from it all?
Dr. Skarupski: The Eastern Shore, specifically to “Gluten Free Bakery Girl” in St. Michaels
 Tony Teano: If you could vacation anywhere in the world, where would you go and why? Where was your last big vacation?
Tony Teano: If you could vacation anywhere in the world, where would you go and why? Where was your last big vacation?
Dr. Skarupski: Just returned from Norway and Belgium. I still need to get to Italy (was heading there in early March of 2020).
Tony Teano: As busy as you are with your job, what renews you when you are away from work?
Dr. Skarupski: The gym is my happy place. I love to exercise. I’ve been playing pickleball for 3 years now and love it.
I was also “friendly-forced” to learn the ukulele this summer, which was really fun.
Tony Teano: I also enjoy playing the ukulele! I’ve noticed that many of your presentations have a musical element. Where did your love of music come from? 
Dr. Skarupski: That comes from learning to play the piano from Sister Mary Williams starting at age 6. I still remember learning Fur Elise and The Blue Danube, and I remember the cupcakes Sister Mary Williams used to give me after my lessons–they didn’t have any frosting, and I always felt sad that the nuns in the convent didn’t have enough money to have frosting–until I learned at her life celebration of her love of licking the frosting off of cupcakes and then repurposing the cupcakes to her piano students!
 Tony Teano: Speechless. Let’s move to the next question…. What is your favorite song?
Tony Teano: Speechless. Let’s move to the next question…. What is your favorite song?
Dr. Skarupski: “Spirit in the Sky” by Norman Greenbaum. I love the lyrics and that driving bass!
Tony Teano: That’s a good one! I love hearing about people’s favorite things…. What is your favorite meaningful quote?
Dr. Skarupski: “And we know that all things work together for good to them that love God, to them who are the called according to his purpose.” Romans 8:28
Tony Teano: Favorite TV show?
Dr. Skarupski: Golden Girls. In fact, Betty White is my backseat driver. 
Tony Teano: That gives me an idea for a few fun last questions. Betty White’s Golden Girls character Rose Nyland once asked this insightful question: “If you could invite any two people over for dinner, living or dead, what would you eat?”
Dr. Skarupski: Sushi and pizza!
Tony Teano: Now, who would those people be and why?
Dr. Skarupski: Larry David and Tina Fey because I love smart, funny, sarcastic people.
Many thanks to Dr. Skarupski for allowing us to get “up close and personal” with her.
Here is a short list of Dr. Skarupski’s research articles in which you may be interested:
- Prevalence of caregiving and high caregiving strain among late-career medical school faculty members: workforce, policy, and faculty development implications
- Factors Influencing Retirement Decisions of Senior Faculty at U.S. Medical Schools: Are There Gender-Based Differences?
- Mentorship Is Not Enough: Exploring Sponsorship and Its Role in Career Advancement in Academic Medicine
- Predictors of aspiration pneumonia in nursing home residents
- Accelerated dysfunction among the very oldest-old in nursing homes
Follow the Office of Faculty Development online: OFD Website; @JHUFacDev; and Instagram: johnshopkinsofd
Learn more about the Faculty Factory: Podcast; Website; and Youtube.
For more information on Writing Accountability Groups, visit: WAGs
For Johns Hopkins employees seeking caregiving resources and support, visit Work Life Programs.
By Anthony L. Teano, MLA
Communications Specialist
Jason R. Falvey, PT, DPT, PhD is an Assistant Professor in the Department of Physical Therapy & Rehabilitation Science and the Department of Epidemiology and Public Health at the University of Maryland School of Medicine. Dr. Falvey is a board-certified geriatric physical therapist and clinician-scientist dedicated to improving aging in place for older adults living with new disability. He is also the Director of the ENhancing Rehabilitation to Improve Community Health (ENRICH) lab, which is designed to reduce participation and mobility inequities among older adults. Dr. Falvey will discuss “Neighborhoods, resilience, and recovery among older adults” at the next scientific seminar being held on Monday, December 4 from 3:30pm – 5:00pm. The seminar will be held at 2024 E. Monument Street, Powe Room, 1-500Q. In person attendance is encouraged. You can also view by registering at https://bit.ly/49tIGLF. Light refreshments will be served.
This seminar is sponsored by: The Matthew Tayback, Sc.D., Memorial Lecture Fund; Center on Aging & Health; Division of Geriatric Medicine and Gerontology; Johns Hopkins Older Americans Independence Center; Epidemiology and Biostatistics of Aging Training Program.
13 people joined the 2023 Johns Hopkins’ Aging & Alzheimer’s Centers’ Walk to End Alzheimer’s Team.
The Baltimore event was held on Saturday, October 28th in Hunt Valley.
Thanks to more than 50 donors to date, we have raised $3,850 for the Alzheimer’s Association, which reflects 77% of our $5,000 goal.
Tax-deductible donations are still being accepted through the end of the year; give here.
Learn more about our team and this cause in a recent COAH blog, which you may find here.
See images from the walk here.
By Anthony L. Teano, MLA
Communications Specialist