We are excited to kick off our COAH Scientific Seminar series for the academic year on Monday, December 5th with Lisa M. Walke, MD, MSHA, AGSF. Dr. Walke is an Associate Professor in Geriatric Medicine and Gerontology as well as Chief in the Division of Geriatric Medicine at the University of Pennsylvania Perelman School of Medicine Penn-Ralston Center. We invite you to join us on Monday, December 5th at 3:30pm for her presentation entitled “Advancing Innovation through Inquiry and Equity” In person attendance is highly encouraged. You may also attend via Zoom by registering at https://bit.ly/3NgHX3h.
You are cordially invited to attend these exciting presentations at 2022 Annual Scientific Meeting of The Gerontological Society of America (GSA) with Johns Hopkins University faculty, staff, fellows, and students; here is a complete list, which you may download and/or print out.
Many thanks to Monique L. Lee, COAH Administrative Coordinator, for compiling this list.
Also, don’t miss COAH Director Dr. David L. Roth’s outstanding address at GSA on Thursday, November 3rd, from 4:30 p.m. to 6:00 p.m. in Room 120-121; titled, “From Stressed Caregivers to Healthy Caregiving: The Implications of Balanced Perspectives and Updated Findings,” Dr. Roth will briefly review updated findings on mortality and inflammatory biomarkers among caregivers.
We wish everyone a great experience at GSA 2022!
By Anthony L. Teano, MLA
Communications Specialist
David L. Roth, PhD, MA is a professor in the School of Medicine, Division of Geriatric Medicine and Gerontology. His research focuses on epidemiological studies of family caregiving, applied statistical analysis, and psychosocial influences on health and healthcare utilization. Dr. David Roth has been at the helm of the center as director for more than a decade. And now Dr. Roth is doing something the likes of which revered leaders, such as George Washington and Cincinnatus, have done—Dr. Roth is stepping down from power and making way for an emerging leader. Let’s learn more about him as a person as well as a professional.
Tell us about your background, education, and path to COAH.
was born and raised in Minot, North Dakota. I have always had a dual fascination with numbers and with how the mind works. I combined those in my undergraduate studies, majoring in both mathematics and psychology at the University of North Dakota. I received a PhD in psychology from the University of Kansas and then took my first faculty position at the University of Alabama at Birmingham. My interests and skills in statistics and data analysis has led me into all kinds of interesting projects and collaborations, including into gerontology. In 2012, I applied for the COAH Directorship and was fortunate to be offered that position.
Your research focuses on applied geriatrics—analyzing data/statistics mostly on family caregivers and on the broader social resources of older adult populations. What about working with numbers appeals to you?
Quantifying behavioral and social factors is a big challenge, but this kind of rigorous measurement is critical for science to advance in these areas. Numbers convey a certain precision, but statistical analysis also incorporates the uncertainty of those numbers and the probabilistic nature of any conclusions we might draw. It’s fascinating to be able to work with colleagues and test hypotheses in research projects that have the potential to greatly improve the lives of older adults and their families.
You have about 270 original peer-reviewed research articles, 229 papers that have been cited 10 or more times, and you are the most cited researcher in the field of applied gerontology according to Google Analytics—currently cited more than 25K times. What advice do you have for junior investigators about becoming a prolific and well-cited researcher in this space?
I think too many researchers with quantitative or data analysis skills are trying way too hard to be as sophisticated as possible in their analytic approaches. This leads to papers with analysis methods that very few colleagues, not to mention the general public, actually understand. I try to emphasize that we want our readers to understand what we are doing and how we are testing our ideas. Let’s not overly complicate things if that is not necessary. Write as clearly as possible, and use conventional analytic methods when they are acceptable. There is no advantage to confusing people, or to conveying a “trust us” attitude on analyses that others don’t comprehend. If colleagues understand your work, they are more likely to cite it, and this increases the potential impact of your work.
You are most well-known for your 2015 paper “Informal caregiving and its impact on health: A reappraisal from population-based studies.” This and other papers led New York Times writers to interview you. Why was this paper so exciting?

This paper challenged a common narrative in family caregiving research that the chronic stress of caregiving results in many serious threats to the caregivers’ health. A few early studies suggested that caregivers have elevated mortality rates, with mortality effects similar to those of smoking. However, many subsequent, large, population-based studies have not only failed to confirm the mortality threat, but actually found that caregivers tended to live longer than many comparison samples of non-caregivers. This has led to an increased attention on the positive aspects of caregiving, how caregiving is a type of social engagement, a form of volunteerism provided within your own family or social network. Caregiving can still be stressful, and caregivers deserve to have services to help them manage their responsibilities, but fortunately, some of the early dire predictions about the physical health consequences of caregiving appear to have been overstated. This paper played a major role in re-balancing the perspectives on the long-term health effects of caregiving.
Last year, you were named the M. Powell Lawton Award recipient from the Gerontological Society of America (GSA). This November, you will deliver the M. Powell Lawton lecture at the GSA Conference in Indianapolis, Indiana, on November 3rd, from 4:30 p.m. to 6:00 p.m. in Room 120-121. Please whet our appetite and give us a teaser about the topic you will discuss and its implications in applied gerontology.
The title of my address is “From Stressed Caregivers to Healthy Caregiving: The Implications of Balanced Perspectives and Updated Findings.” In the talk, I will briefly review the mortality findings discussed above and also review similar findings on inflammatory biomarkers. In both areas, the caregiving literature shows a bias pattern that is often found in other areas—particularly in the social and behavioral sciences, where early studies with relatively small sample sizes and alarming results are widely cited–whereas numerous subsequent studies with larger samples and better methods that don’t support the original alarming results are usually given much less attention. Science slowly corrects these biases over time, but it shouldn’t take as long as it often does.
I heard you say that one of your favorite quotes about leadership is from Lao Tsu: “To lead people, walk beside them… As for the best leaders, people do not notice their existence. The next best, people honor and praise. The next, people fear; and the next, people hate…. When the best leader’s work is done, people say, ‘We did it ourselves!’” Tell us about a few examples in your personal or professional life where you think you lived up to this value.
As the Director of the Center on Aging and Health, I have tried to expand our breadth and to recruit and retain outstanding investigators. I have then tried to mostly stay out of their way as they do their exceptional work. They did do it themselves. If I had some small role in creating an environment where that could happen, and where they could expand their collaborative networks, then I have done a good job as a leader, but it’s really more as a facilitator than anything else.
This October, COAH turns 25, and you have been at its helm for more than a decade. What are a few of the most significant things to have developed at COAH over the past 10 years?
It’s hard to give a short answer to that. We have grown and expanded, while maintaining and advancing our historical strengths. We are well-known for our work on frailty, and rightfully so. That group continues to thrive and improve the lives of many older adults. We have established about 8 distinct working groups. We are much more active in analyzing national databases and examining trends in healthcare utilization using Medicare claims data as part of our Linked Administrative Data Resource (LADR). We have become very active in work on mobility, on international approaches to harmonizing cognitive aging data, on sensory changes associated with aging, and this is just a small sampling of the many innovative projects and collaborations that are ongoing. I apologize to the many productive and outstanding scientists we have whom I have failed to mention in this brief response.
If you didn’t have the position/career you’re in now, what would you be doing instead?

That’s a scary question. I have been blessed to have a rewarding and stimulating career. My biggest fear is boredom, but that never happens in my job. Research is always challenging and changing. It keeps you fresh and always striving to improve. I’m afraid that a lot of other careers, where you do similar things over and over again, would bore me.
Recently, you decided to step down as director of COAH. What will you do next?
That’s a good question. I will still collaborate, but spend more time away from work and enjoying the great outdoors. I love nature and being in the countryside.
Dr. Roth, this is an amazing track record of success! Thanks for sharing your thoughts on these professional matters.
Now, let’s turn to who you are when you’re not at work—and get a glimpse into your private world.
What is your earliest memory? How does it make you feel?
Pulling up in a pickup truck with my Dad to the new house my parents bought when I was 3 years old. It is a warm memory.
Is there any fun fact to know and tell you’d like us to know about your home life, family, where you grew up, etc.?
I came from a great family. A strong Catholic family. My parents were married for over 63 years, until my Dad passed away a few years ago in 2020 at the age of 90. My Mom is 86 and is still with us. She has a great sense of humor, and it is very fun to visit her, which I do every chance I get. Also, I have 3 great sisters, and a brother, too.

It sounds like your parents may have some secrets to healthy aging. With your expertise in this field, what have you observed about them to this extent?
They’re both from strong, midwestern farming families. They learned to work hard at an early age and to also take good care of themselves. When you were out on the farm 70-80 years ago, you had to be self-sufficient. They mastered that. They lived fairly simple, healthy lives, and had active lifestyles, not necessarily from exercise classes, but from everyday physical activities.
Tell us about when you think you first became aware of aging as an important health topic.
In graduate school, I received training in both neuropsychology and behavioral medicine. Both fields alerted me to the importance of aging, and to the importance of disease prevention and building optimal functioning over time. Then, when I started doing more collaborative work as an applied statistician, I became very impressed with the social dimensions of aging, the advantages of having a strong family, a robust social network, and the perils of social isolation. These interests grew and merged over time to create the scholar I am today.
What are some of your favorite, ordinary guilty pleasures?
-

Jackson and Dr. Roth on the Magothy River TV show… I’m sure I’ve seen every Seinfeld episode multiple times, and still sometimes watch those reruns even now.
- Meal you cook… I love roasted duck, with acorn squash, a good green veggie, and an excellent bottle of red wine.
- Daytrip getaway destination… I take my boat out on the Magothy River frequently. There is a little island that I pull up to and let my dog swim and play. I have named it “Jackson island” after my dog.
- Quote… “The perfect is the enemy of the good.” Most attribute this to Voltaire, and I really agree with it. If we try to be perfect, we fail. We should try to be good, and always try to improve, but, as humans, we can never achieve perfection.
What is the top item on your bucket list?
To travel a lot more and see places in the world that I haven’t visited yet.
Where would you vacation if money was not an issue?
I have this fantasy to go camping in the Himalayas.
What advice did you receive as a young person that has served you well?
Finish what you started. Don’t quit on people. You want others to know that they can rely on you.
What advice do you have for young people today?
Be true to yourself. Try different things, partly to discover what you are good at, and what you enjoy doing, and then figure out a way to get paid to do those things as part of your career.
In my humble opinion, Dr. Roth treats the COAH team as members of an extended family brought together around core values of excellence and a commitment to inquiry into matters impacting older adults and their caregivers. Since COVID-19, he has found creative ways to bring his team together—whether it is for an occasional luncheon when pandemic conditions permitted, or virtually for periodic “COAH Coffee Hour” Zoom meetings to just banter and share what’s going on as real people. Ukulele, guitar, and even a xylophone was involved. To me, a hallmark of Dr. Roth’s leadership has been to cultivate cohesive camaraderie and to facilitate creative connections among passionate people whom he celebrates. He has consistently nominated COAH team members for various awards. As he gracefully vacates the director position, it is reassuring to know Dr. Roth is not leaving this wonderful community of people that he has mentored and nurtured, but rather he is becoming a different kind of collaborator and peer—and Dr. Roth will most certainly remain a champion of and among COAH champions.
You may also be interested in the following blogs by or about Dr. Roth:
- David L. Roth’s Recent Latent Variable Study Identifies Possible Inhibitory Pathway Contributing to Long-Term Caregiver Stress (Sept., 2022)
- Family Caregiving: An Essential Resource for Older Adults (Nov., 2021)
- David L. Roth to Receive the 2021 M. Powell Lawton Award from the Gerontological Society of America (Oct., 2021)
By Anthony L. Teano, MLA
Communications Specialist
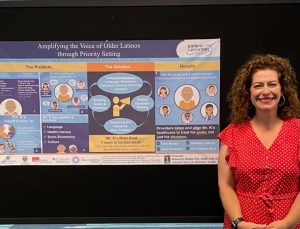
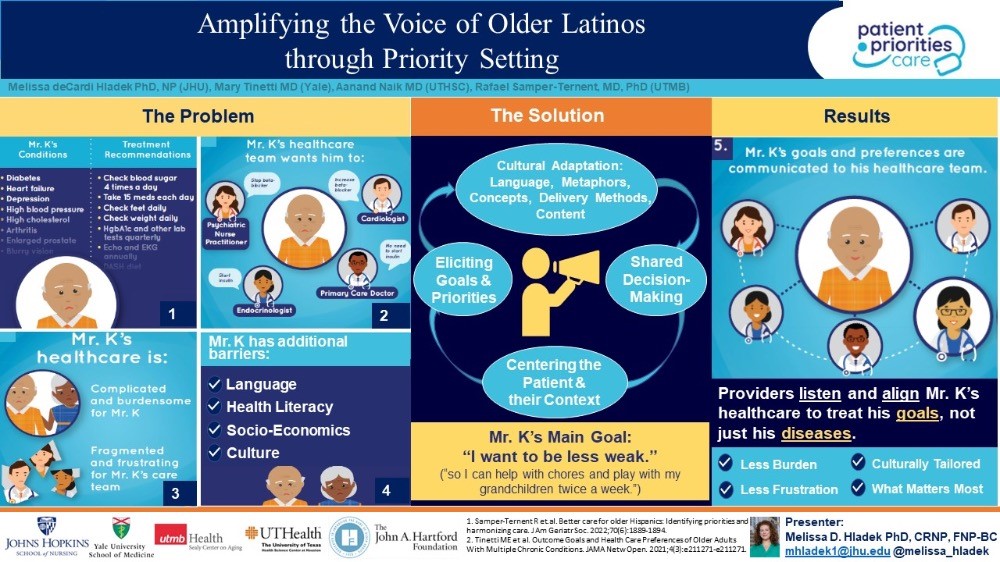
Dr. Melissa deCardi Hladek is an Assistant Professor with the Johns Hopkins University School of Nursing, and she is well-known as a researcher-clinician with work focusing on how stress, self-efficacy resilience, and sociocultural factors influence the biology of aging, chronic disease, and frailty. Her research goals are to further understand the role of stress, coping and social determinants of health in aging and develop novel strengths-based, person-environment strategies and policies to mitigate these effects and center the patient’s voice in modern healthcare. Dr. Hladek is a regular participant and collaborator among several COAH workgroups, including the Frailty Working Group, and a Research Education Core grant awardee from the Johns Hopkins Older Americans Independence Center. As an FNP, Dr. Hladek has worked with vulnerable populations experiencing homelessness and incarceration in both rural and urban settings with primarily Spanish-speaking communities. She is the president-elect for the National Association of Hispanic Nurses (NAHN)-DC Metro Chapter and advisor for the Latinx Health Advisory Group at Johns Hopkins School of Nursing.
Earlier this year, she presented a poster at NAHN’s annual conference on “Amplifying the Voice of Older Latinos through Priority Setting,” which serves as the basis of her blog that follows, and which we are delighted to share with you during National Hispanic American Heritage Month 2022. Many thanks to Dr. Hladek for sharing the wisdom of her research on this topic with us now.
 This blog post really comes out of my and my colleagues’ deep desire to meet the healthcare needs of older Latinos in our communities. Latinos currently represent 19% of the total US population, and the number of adults over the age of 65 identifying as Hispanic is projected to double over the next decade. Older Latinos have the highest percentage of any racial or ethnic group living below the poverty line (19.5%), with more than 40% having not completed high school. These socio-economic disparities exacerbate the existing high chronic disease burden and disability experienced by older Latino adults. Multiple studies have identified barriers around language, culture, and healthcare literacy contributing to these poorer health outcomes. Currently, 5.8% of all physicians and 8.4% of all nurses identify as Hispanic or Latino, which puts a disproportionate burden on these providers to deliver culturally concordant care.
This blog post really comes out of my and my colleagues’ deep desire to meet the healthcare needs of older Latinos in our communities. Latinos currently represent 19% of the total US population, and the number of adults over the age of 65 identifying as Hispanic is projected to double over the next decade. Older Latinos have the highest percentage of any racial or ethnic group living below the poverty line (19.5%), with more than 40% having not completed high school. These socio-economic disparities exacerbate the existing high chronic disease burden and disability experienced by older Latino adults. Multiple studies have identified barriers around language, culture, and healthcare literacy contributing to these poorer health outcomes. Currently, 5.8% of all physicians and 8.4% of all nurses identify as Hispanic or Latino, which puts a disproportionate burden on these providers to deliver culturally concordant care.
There is an urgent need to develop care pathways for older Latino adults with multimorbidity that centers their experience, and that values in a systematic way and aligns care plans with their priorities. When I think of solutions for these very complicated factors, one evidenced-based approach that immediately comes to mind is entitled “Patient Priorities Care” (PPC). Providing care for older adults with multiple chronic conditions (MCCs) is challenging because of uncertainty of treatment benefits, burden of managing multiple conditions, and inapplicable or conflicting disease-specific guidelines traditionally used to make care decisions. These individuals receive care that is often burdensome, fragmented, and not focused on what matters most to them. In this complicated landscape, shared decision-making, accounting for patient preferences, is the preferred method of decision-making.1,2 Whereas many guidelines focus on disease specific outcomes, older adults often prioritize maintaining independence and quality of life.3 Consequently, obtaining patient preferences facilitates fundamental healthcare system shifts toward “value-based healthcare.”4
As a result of this growing problem in the primary care management of older adults with MCCs, the John A. Hartford Foundation (JAHF) and the Patient Centered Outcomes Research Institute elicited perspectives on how to address these problems from over 150 individuals and dozens of organizations representing patients, family caregivers, health systems, payers, clinicians, and experts in practice change and information technology.1 The consensus solution was entitled “Patient Priorities Care,” a continuous process that begins when patients identify their health priorities. These priorities are used in decision-making among patients and clinicians, centering the patient and their values in the care alignment decision-making process. The work informs the “What Matters” of JAHF’s Age-Friendly Health Systems and, the patient goals-based metrics emanating from JAHF’s Person-Reported Outcome Measures initiative supports uptake of PPC as well. PPC was shown to reduce treatment burden and other metrics related to improved health outcomes in a non-randomized clinical trial (N=366) of older adults with multi-morbidity.5,6 Additionally, we conceptualize centering the patient’s preferences as an integral step in acting upon social determinants of health data and other health equity priorities for older adults, which circles us back to the Latino community.7
PPC was not initially designed with the unique needs of older Latinos in mind. We propose that using an ecological validity model that incorporates an understanding of the whole person, including their lived environment, to culturally tailor PPC will greatly benefit this community. There are eight dimensions of the Ecological Validity Model that could help inform a PPC adaptation including: language; persona (circumstances that commonly affect Latinos); metaphors; content; concepts; goals; methods; and context. Based on my and my colleagues’ lived experience and work within this community, we also acknowledge the heterogeneity of the Latino community and both the religious and cultural belief systems—like “familismo” and “personalismo”—in order to understand healthcare priorities among older Latino adults. In other words, “person-centered” can have a more expanded meaning to include family members or caregivers in the Latino context.
It is of critical importance to account for the unique strengths and health disparities attributed to existing social determinants of health when adapting interventions, like PPC, to the older Latino adult population. A PPC adaptation for the Latino population holds promise to amplify the patient’s voice, improve health outcomes and promote health equity.
References:
- Cooper Z, Courtwright A, Karlage A, Gawande A, Block S. Pitfalls in communication that lead to nonbeneficial emergency surgery in elderly patients with serious illness: Description of the problem and elements of a solution. Ann Surg. 2014;260(6):949-957. doi:10.1097/SLA.0000000000000721
- Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140(1):54-59. doi:10.7326/0003-4819-140-1-200401060-00012
- Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061-1066. doi:10.1056/NEJMSA012528
- Mooijaart SP, Carpenter CR, Conroy SP. Geriatric emergency medicine-a model for frailty friendly healthcare. Age Ageing. 2022;51(3). doi:10.1093/AGEING/AFAB280
- Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient Priority-Directed Decision Making and Care for Older Adults with Multiple Chronic Conditions. Clin Geriatr Med. 2016;32(2):261-275. doi:10.1016/J.CGER.2016.01.012
- Tinetti ME, Naik AD, Dindo L, Costello DM, Esterson J, Geda M, et al. Association of Patient Priorities–Aligned Decision-Making With Patient Outcomes and Ambulatory Health Care Burden Among Older Adults With Multiple Chronic Conditions: A Nonrandomized Clinical Trial. JAMA Intern Med. 2019;179(12):1688-1697. doi:10.1001/JAMAINTERNMED.2019.4235
- Samper-Ternent R, Tinetti M, Jennings LA, Wong R, Arney J, Naik AD. Better care for older Hispanics: Identifying priorities and harmonizing care. J Am Geriatr Soc. 2022;70(6):1889-1894. doi:10.1111/JGS.17748
By Melissa deCardi Hladek, PhD, MSN, RN, CRNP, FNP-BC




