An old adage goes something like this: “Growing old is not for the faint of heart.” Perhaps there’s something else about the aging human condition at parity with this wisdom: caregiving is both challenging and rewarding. And perhaps listening to caregiver experiences individually and as an aggregate can help us prepare for a culture and society where aging and caregiving can be less challenging and more rewarding.
Now is the time to do so.
According to Aging Care’s Caregiver Statistics, in 2020, the AARP Public Policy Institute and the National Alliance for Caregiving reported that 53 million Americans are providing unpaid care to family and friends, and family caregivers provide an average of 23.7 hours of care each week—and if they cohabitate, the number of hours increases to 37.4 hours weekly.
Baby boomers are getting older and living longer, and the Population Reference Bureau projects the number of Americans over the age of 65 will practically double between 2018 to 2060, from 52 million to 95 million people. Additionally, given the fact that many older adults develop chronic conditions as they age, combined with the scarcity of affordable care, we can only expect the number of “informal” or “family caregivers” to grow over time, especially as older adults overwhelmingly desire to age in place, in their own homes.
 Many quantitative studies have examined the health impact of providing care on those who care for family and friends, but few qualitative studies looked into the nuances of how they think, feel, and perceive their experience as a caregiver. To better understand and support them, that’s precisely what Drs. Marcela Blinka, Orla Sheehan, and David L. Roth from JHU’s COAH investigated along with colleagues from the University of Vermont and the University of Alabama at Birmingham. The results of the study, “Family caregivers emphasize patience and personal growth: a qualitative analysis from the Caregiving Transitions Study,” was published in Age and Ageing in February, 2022.
Many quantitative studies have examined the health impact of providing care on those who care for family and friends, but few qualitative studies looked into the nuances of how they think, feel, and perceive their experience as a caregiver. To better understand and support them, that’s precisely what Drs. Marcela Blinka, Orla Sheehan, and David L. Roth from JHU’s COAH investigated along with colleagues from the University of Vermont and the University of Alabama at Birmingham. The results of the study, “Family caregivers emphasize patience and personal growth: a qualitative analysis from the Caregiving Transitions Study,” was published in Age and Ageing in February, 2022.
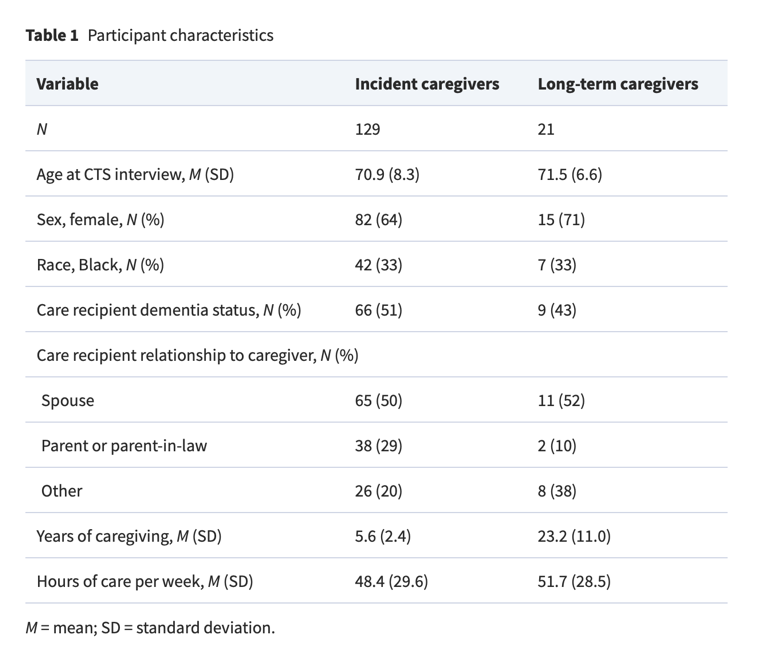
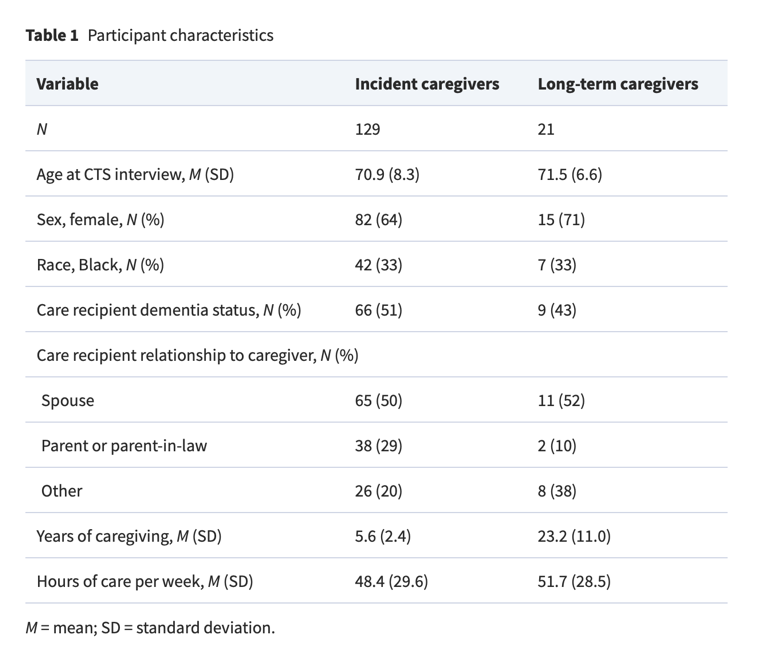
They examined 251 responses to an open-ended question on the Caregiving Transitions Study—an ancillary of the Reasons for Geographic and Racial Differences in Stroke study—that gathers data about family caregiving and its effect on family caregivers: “Is there any other information that you can think of about your experience in being a caregiver that we should know about or you think might be beneficial to the study?” Upon a thorough review of the answers, the team identified four themes:
- Cultural/family expectations
- Growth opportunities
- Reciprocity
- Stressors/challenges and recommendations
These caregivers provided about 50 hours of care per week, well above the national average. Most of the caregivers were White women in their 70s providing care to a spouse with dementia. For some, it was their second turn at caregiving, having already cared for a parent. Reflecting a few of the themes above, here is a sample of moving, heart-felt, and all-too-real responses from caregivers in their own words:
- “I promised my father-in-law that I would do whatever it takes to not put [my mother-in-law] in a nursing home.”
- “It is something you have to do from the heart, if your heart is not in it you will not be able to stick with it… remember that when things get tough, and your loved one says things that hurt you, you have to realize it’s not that person saying things to you, it is their disease.”
- “I do not like the word ‘caregiver.’ We are married. I do not get paid. I do what I do out of love.”
- “‘We have a faith-based view that places great importance on honoring your parents.”
- “You treat them the way that you would want to be treated because… one of these days we will all need help.”
- “[Even though] there are a lot of resources out there to help… programs are not available to everyone so we have to pay out of pocket which I am not capable of doing.”
- “If there was a way to get a mental break from everything for just a little while it would help a lot.”
- “Very difficult emotionally [and] I also feel like a prisoner.”
- “There is a time period where you have to come to the realization that this is the way it is and do the best you can.”
- “He refuses to let me [help him], because he doesn’t want to be a burden to me… I have a feeling that many care-recipients feel the same way.”
Many individuals who have been caregivers may identify with these themes. Essential to understanding the enormity of it all is the reality that the caregiving experience is in fact paradoxical. It isn’t all easy or fun, and it can be anguishing sacrifice. But sometimes, it has a silver lining, too, and encompasses “both/and.” Caregiving can push people to grow in ways previously unimagined and spur deep human growth and awareness. This realization can teach us to be aware of what we must do to anticipate and prepare for an aging society that relies upon their informal and family caregivers. What do they need right now? How can interventions help people become better, healthier caregivers? What resources need to be developed to support them?
The insights from this qualitative review are useful and impactful because “The projected need for informal caregiving for older adults is expected to outpace the number of available caregivers dramatically in the next decade. As such, caregivers’ readiness and/or burden in their role are of great importance to an ever-increasing proportion of the population.”
The research team’s key takeaways from the study were:
- Caregiving was viewed as an unquestioned obligation, repayment of benefits provided by the family member, acts of love, or the fulfilment of promises.
- Opportunities for growth and reciprocity were the important aspects of the caregiving experience.
- Caregivers experienced lifestyle changes, financial burdens, and desire for more support in their role.
Dr. Blinka, the first author, wrote: “Informal caregivers are essential to an aging society, especially as there is an increasing emphasis to allow older adults to age in place. Our findings show that caregivers can meet the challenges of caregiving by finding meaning, engaging in mutual support with the care recipient and identifying opportunities for growth. A more comprehensive understanding of the caregiving experience can help inform future interventions as well as provide guidance for how individuals and systems can most effectively support caregivers in fulfilling their roles.”
Dr. Blinka is available for interviews and comments.
By Anthony L. Teano, MLA
Communications Specialist
 Tom Cidav – New hire: Biostatistician (April 2020)
Tom Cidav – New hire: Biostatistician (April 2020)






 Many quantitative studies have examined the health impact of providing care on those who care for family and friends, but few qualitative studies looked into the nuances of how they think, feel, and perceive their experience as a caregiver. To better understand and support them, that’s precisely what Drs. Marcela Blinka, Orla Sheehan, and David L. Roth from JHU’s COAH investigated along with colleagues from the University of Vermont and the University of Alabama at Birmingham. The results of the study, “
Many quantitative studies have examined the health impact of providing care on those who care for family and friends, but few qualitative studies looked into the nuances of how they think, feel, and perceive their experience as a caregiver. To better understand and support them, that’s precisely what Drs. Marcela Blinka, Orla Sheehan, and David L. Roth from JHU’s COAH investigated along with colleagues from the University of Vermont and the University of Alabama at Birmingham. The results of the study, “