It is with great pleasure that we celebrate the achievements and contributions of Brian Buta, MHS, and name him our Winter 2024 COAH Champion. As you probably already know, Brian is the Project Administrator with the Center on Aging & Health, and he plays a critical role in the daily operations of the center. In addition to shepherding through many of COAH’s goals and objectives with adept management and excellent interpersonal skills, you may be interested to know that Brian is also a keen researcher in the etiology and assessment of frailty, in interventional and translational studies among older adults, and in health promotion and dissemination. Please enjoy this opportunity to get to know him better as an esteemed colleague, and, moreover as a fun, kind person.
Tony Teano: Let’s start off with a few questions about your work. Tell us about your background, education, and path to COAH.
Brian Buta: I am a born-and-raised resident of Baltimore. I grew up in Baltimore County and graduated from Goucher College where I majored in Sociology and took a lot of music courses. After graduation, I was fortunate to land a part-time job as a research assistant with anthropologist Dr. Sidney Mintz, while also waiting tables at a local country club. I worked in this position for nearly two years, before accepting a position as a research assistant in the Center on Aging and Health. Besides a great affinity for my grandparents, I did not know much about aging or aging research but I had grown curious while working with Sid. He was already in his 80’s when I started assisting him with his research articles, books, and lectures. Sid was kind, funny, prolific, and producing fascinating work as an octogenarian and it made me reflect on the contrast between his later life activities and the stereotypical notions about what it looks like to grow old.
Tony: Tell us about your job.
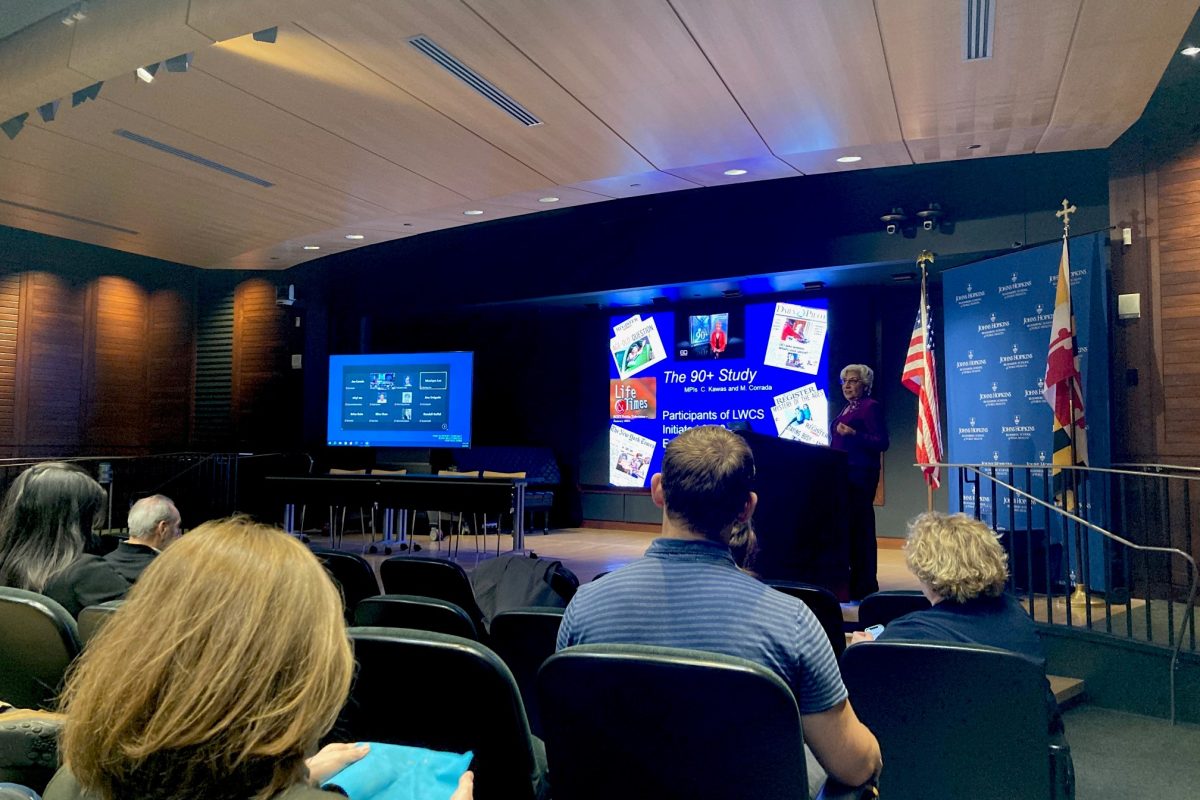
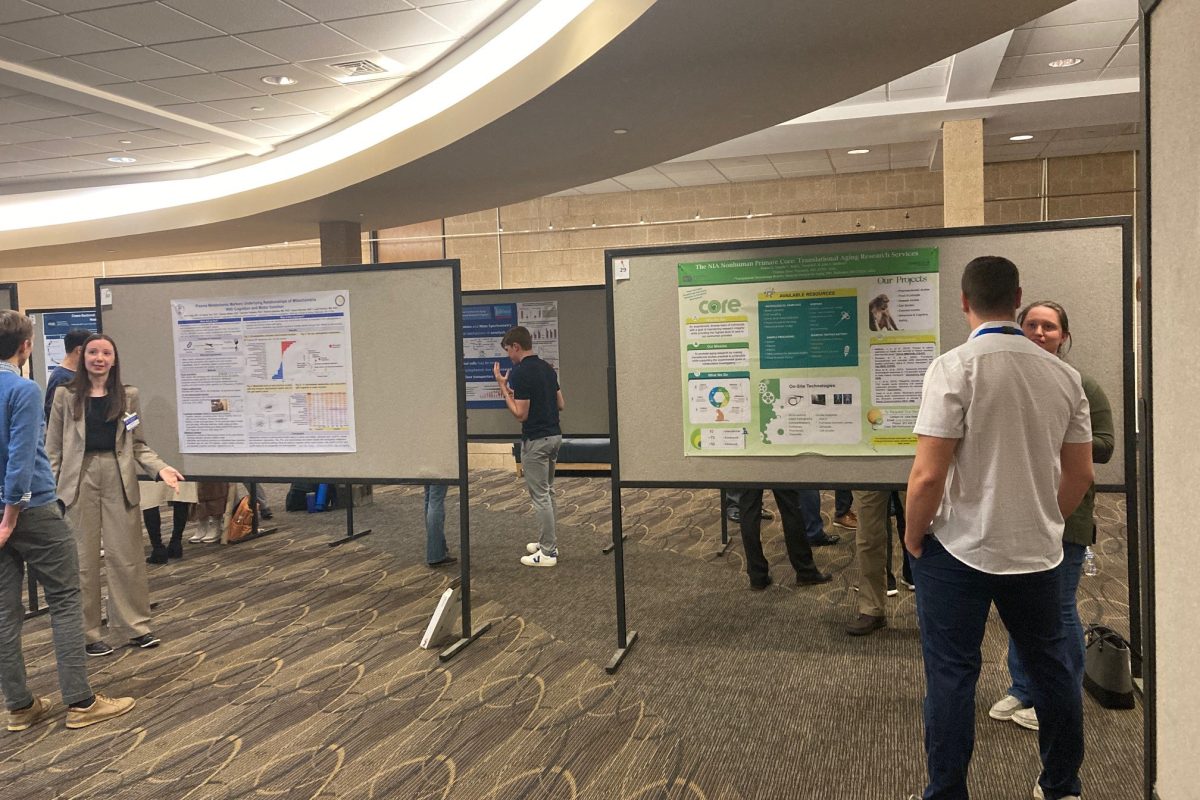
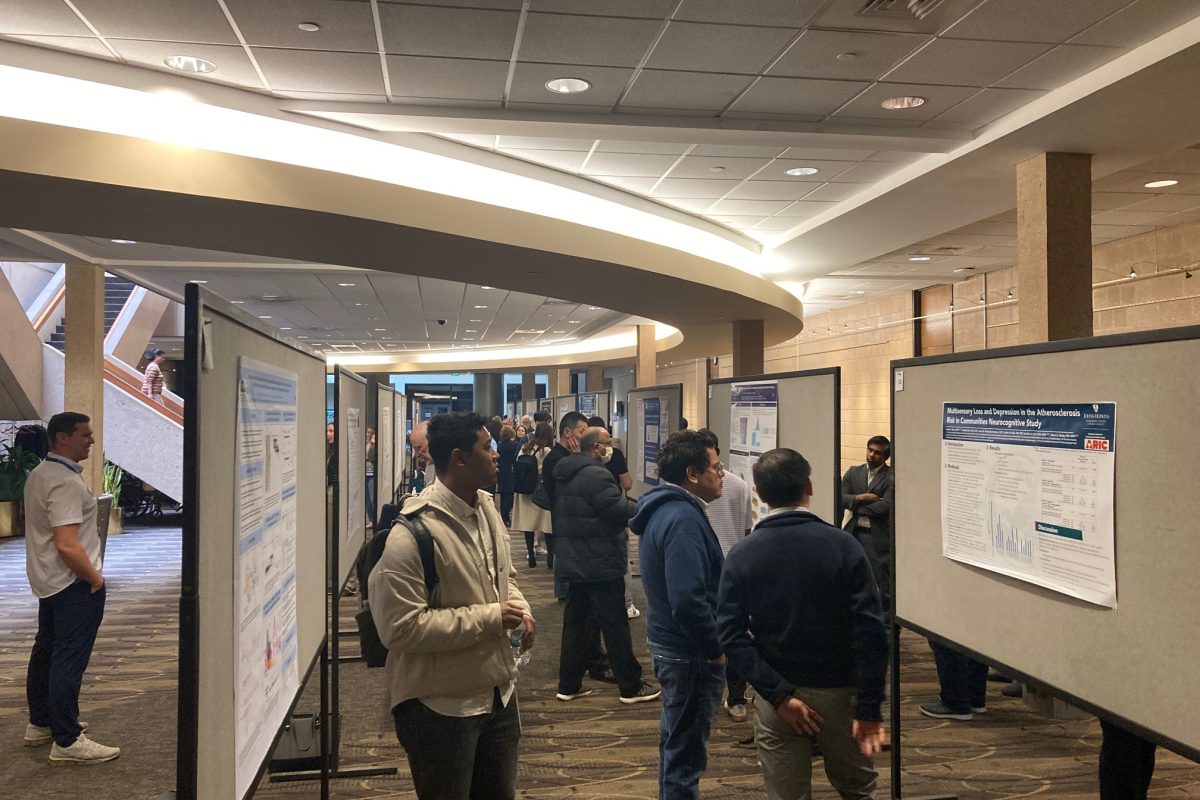
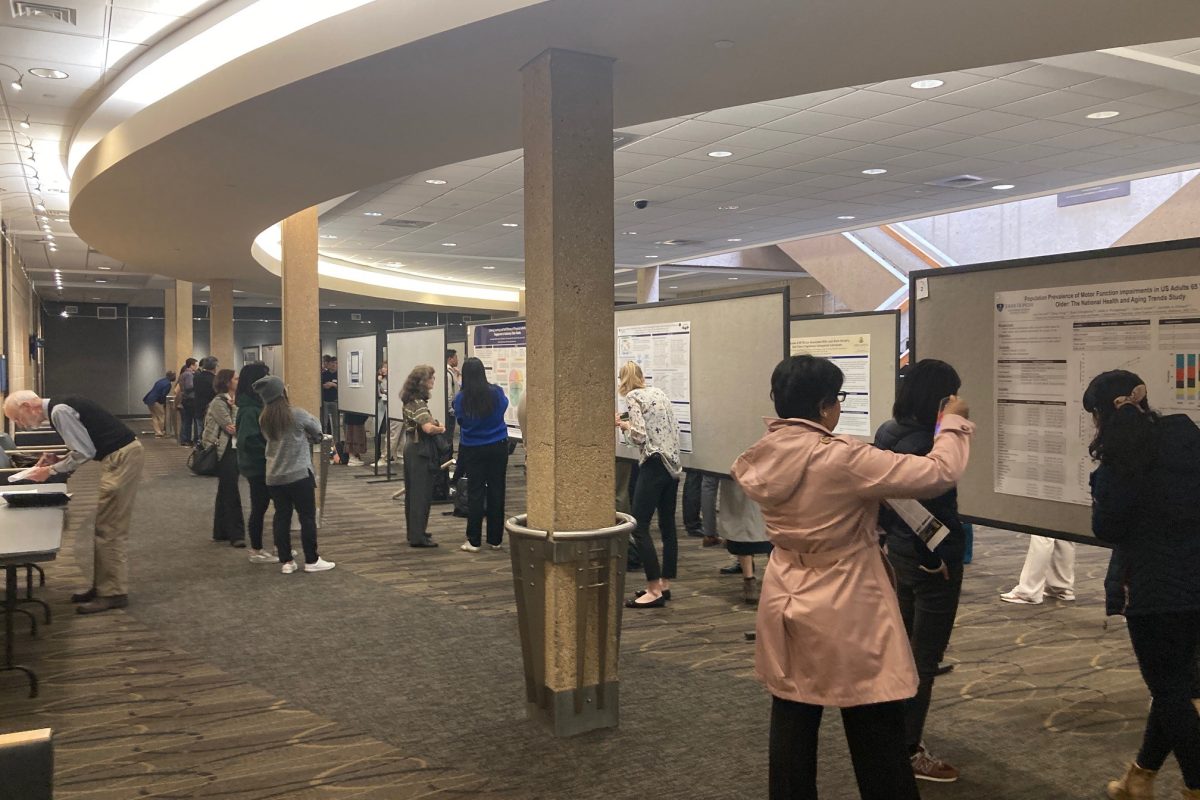
Brian: I am a project administrator for the Division of Geriatric Medicine. In this role, I provide management and oversight for several divisional research programs and grant awards. I am the center administrator for the multidisciplinary Center on Aging and Health on the JHMI campus; and the administrator for the frailty-focused Claude D. Pepper Older Americans Independence Center (OAIC; P30 Grant), the Study of Physical Resilience and Aging (SPRING; UH2/UH3 Grant), and the Epidemiology and Biostatistics of Aging (EBA)Training Program (T32 grant). Across these programs, I provide staff supervision, financial and operational tracking, grant writing support, regulatory support, study implementation, and progress/accountability management. I am also grateful to participate in research activities, including study design, manuscript writing, conference presentations, and serving as the facilitator for the Frailty & Multisystem Dysregulation Working Group.
Tony: What is the best part of your job?
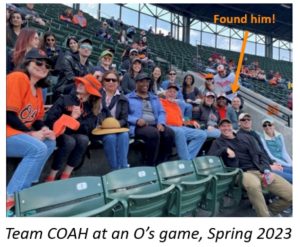
 Brian: The people I get to work with are what makes my job special to me. I have a core team of wonderful mentors and colleagues throughout the Division. Through the programs named above (and more), I get to work with talented and inspiring faculty, staff, fellows, and students from across the School of Medicine, the broader University, and beyond. For example, through our frailty working group, I have the opportunity to collaborate with aging researchers from across the U.S. and internationally. Bringing people together from different disciplines, cultures, and life experiences is extremely valuable to the pursuit of high-quality science, and I am thrilled be part of a team with an incredible breadth and depth of aging science knowledge.
Brian: The people I get to work with are what makes my job special to me. I have a core team of wonderful mentors and colleagues throughout the Division. Through the programs named above (and more), I get to work with talented and inspiring faculty, staff, fellows, and students from across the School of Medicine, the broader University, and beyond. For example, through our frailty working group, I have the opportunity to collaborate with aging researchers from across the U.S. and internationally. Bringing people together from different disciplines, cultures, and life experiences is extremely valuable to the pursuit of high-quality science, and I am thrilled be part of a team with an incredible breadth and depth of aging science knowledge.
Tony: You are part of COAH’s Frailty Working Group and also Frailty Science’s team. Why did you decide to focus on frailty?
Brian: I basically fell into frailty research by working at COAH and with the OAIC. I started mostly on the administrative/progress management side, but became greatly interested in the science of aging-related vulnerability and heterogeneity. I am passionate about rigorous science in this area, and about strategies to best share with older adults and their families what we learn through our research that can support their healthy aging.
Tony: What papers are you most known for or most proud of in these areas?
Brian: Most of my research has focused on physical frailty among older adults. My first publication in this area was as a co-author on a study that examined the prevalence of frailty among older adults in the United States, published in the Journal of Gerontology: Medical Sciences, titled Frailty in Older Adults: A Nationally Representative Profile in the United States (Bandeen-Roche et al., 2015). This work was followed by a review project on frailty assessment instruments and their uses to date in the literature—a project that took a couple years to complete; under the mentorship of Drs. Ravi Varadhan, Jeremy Walston, Qian-Li Xue, and Karen Bandeen-Roche, we published in Aging Research Reviews: Frailty Assessment Instruments, (Buta et al., 2016). More recently, I am proud of the concept and design paper on the Study of Physical Resilience and Aging (SPRING): A conceptual framework, rationale, and study design (Walston et al., 2023) that was published in the Journal of the American Geriatrics Society.
Tony: What is the most interesting or astonishing finding from your research?
Brian: I am fascinated by the challenge of trying to reconcile the concept of frailty and its importance for the clinical care of older adults with the fact that people, in general, do not like the terms “frail” or “frailty” and do not want to think of themselves as frail. How do you talk to patients about frailty when the word itself can be off-putting in its inherent notions of weakness and failing? A simple response is to pick a new term! But this is an ongoing issue to be figured out in this field of research.
Tony: What research are you currently working on?
Brian: I work on many different projects, so every day is a bit different. Key tasks at present include overseeing the final phase of the SPRING resilience grant; preparing the annual progress report for the frailty-focused OAIC; and managing fellowship recruitment activities for the Epidemiology & Biostatistics of Aging training program. I also have ongoing research studies that explore the associations of self-reported health (SRH) and frailty in a community-dwelling population, as well as SRH and physical resilience among patients undergoing clinical procedures.
Tony: Last year, you won a Diversity Innovation Grant award to foster the recruitment of diverse older adults to research studies. Tell us about this initiative and why you thought it was important to do.
 Brian: I think this is a hugely important topic. Older adults and persons from minoritized populations are disproportionately affected by the burden of diseases and health problems, but these groups have been historically and vastly under-represented in research studies. This disconnect can mean that the strategies and treatments developed through research to improve health may not be meet the critical needs of those who are most vulnerable. So, we aimed to equip frontline research staff and research managers at Hopkins with knowledge on optimal strategies for the recruitment of diverse older adults into research, with the big-picture goal to improve enrollment of underrepresented older participants–including individuals from racial/ethnic minority groups and individuals from LGBTQ+ communities–into research studies and clinical trials. About 25 research staff completed a set of online courses in the spring of 2023. At the start of the program, only 25% rated themselves as moderately familiar with strategies that may contribute to the successful recruitment of older, underrepresented persons into research studies; the other 75% rated themselves as somewhat familiar, slightly familiar, or not at all familiar. By the end of the 2-month training program, we saw a notable shift: 30% rated themselves as extremely familiar and 70% as moderately familiar with relevant strategies. We hope to hold this training again soon. Also related to this topic, I worked with colleagues in Medicine, Nursing, and Public Health to write a book chapter on the social determinants of physical frailty that highlights the numerous societal-level factors that contribute to health declines among older persons.
Brian: I think this is a hugely important topic. Older adults and persons from minoritized populations are disproportionately affected by the burden of diseases and health problems, but these groups have been historically and vastly under-represented in research studies. This disconnect can mean that the strategies and treatments developed through research to improve health may not be meet the critical needs of those who are most vulnerable. So, we aimed to equip frontline research staff and research managers at Hopkins with knowledge on optimal strategies for the recruitment of diverse older adults into research, with the big-picture goal to improve enrollment of underrepresented older participants–including individuals from racial/ethnic minority groups and individuals from LGBTQ+ communities–into research studies and clinical trials. About 25 research staff completed a set of online courses in the spring of 2023. At the start of the program, only 25% rated themselves as moderately familiar with strategies that may contribute to the successful recruitment of older, underrepresented persons into research studies; the other 75% rated themselves as somewhat familiar, slightly familiar, or not at all familiar. By the end of the 2-month training program, we saw a notable shift: 30% rated themselves as extremely familiar and 70% as moderately familiar with relevant strategies. We hope to hold this training again soon. Also related to this topic, I worked with colleagues in Medicine, Nursing, and Public Health to write a book chapter on the social determinants of physical frailty that highlights the numerous societal-level factors that contribute to health declines among older persons.
Tony: What is your best advice about career development?
Brian: Read carefully, listen carefully, and make time to deeply understand the work and how all members of the team are contributing to the bigger goal.

Tony: Turning to your life outside of work, tell us about your hobbies. What renews you?
Brian: I enjoy running and playing the guitar. I love taking trips and playing board games with my family. I also like doing crossword puzzles, sudoku, and Wordle.
Tony: Now for a short list of your favorites…. Let’s go with songs/performers, board games, and your favorite meal that you cook.
Brian: Two all-time favorite songs are Here Comes The Sun by The Beatles, and Heroes by David Bowie. My favorite board games are Sequence and Scrabble. Can we get a divisional Sequence tournament going? And I enjoy cooking Chicken Marbella—a neighbor shared this unique dish with us and it’s delicious and easy to make.
Tony: I leave it to our fearless leader, Dr. Schrack, to confer with Dr. Boyd about a divisional board game tournament… Meanwhile, what is your best advice on aging well?

Brian: There will always be stress in life; the goal is not to avoid stress, but to learn to manage it as best as we can and hopefully with the support of others.
Tony: If you could go anywhere in the world, what place would you like to visit and why?
Brian: The Galapagos Islands would be amazing. I’d also love to visit more national parks. Yosemite is one of the most amazing places I have been to, and I would love to make it to Yellowstone in the future.

Tony: I believe you were in a band. For our last interview topic, please tell us all about that part of your life.
Brian: Music has played a special role in my life. I have played guitar and written songs since I was in middle school, and I continue to play, write, and record as my main creative outlet. I played in different rock bands in my teens and twenties, and I still occasionally play out with friends.
We thank Brian for making time for this interview, and for his many on-going efforts and new innovations at COAH. As you can see, Brian is a great team-player, an inspirational leader, and an all-around wonderful person. We are lucky to have him. And when we say he’s a rock star, we mean it!
Learn more about his specialty in frailty and resiliency among older adults at the Frailty Science website—yet another Geriatrics group in which he plays a critical role—where you can find many blogs he wrote, as well as explore the overall content, podcasts, guidance on selecting a frailty assessment instrument, and more helpful information.
By Anthony L. Teano, MLA
Communications Specialist







 Brian: The people I get to work with are what makes my job special to me. I have a core team of wonderful mentors and colleagues throughout the Division. Through the programs named above (and more), I get to work with talented and inspiring faculty, staff, fellows, and students from across the School of Medicine, the broader University, and beyond. For example, through our frailty working group, I have the opportunity to collaborate with aging researchers from across the U.S. and internationally. Bringing people together from different disciplines, cultures, and life experiences is extremely valuable to the pursuit of high-quality science, and I am thrilled be part of a team with an incredible breadth and depth of aging science knowledge.
Brian: The people I get to work with are what makes my job special to me. I have a core team of wonderful mentors and colleagues throughout the Division. Through the programs named above (and more), I get to work with talented and inspiring faculty, staff, fellows, and students from across the School of Medicine, the broader University, and beyond. For example, through our frailty working group, I have the opportunity to collaborate with aging researchers from across the U.S. and internationally. Bringing people together from different disciplines, cultures, and life experiences is extremely valuable to the pursuit of high-quality science, and I am thrilled be part of a team with an incredible breadth and depth of aging science knowledge. Brian: I think this is a hugely important topic. Older adults and persons from minoritized populations are disproportionately affected by the burden of diseases and health problems, but these groups have been historically and vastly under-represented in research studies. This disconnect can mean that the strategies and treatments developed through research to improve health may not be meet the critical needs of those who are most vulnerable. So, we aimed to equip frontline research staff and research managers at Hopkins with knowledge on optimal strategies for the recruitment of diverse older adults into research, with the big-picture goal to improve enrollment of underrepresented older participants–including individuals from racial/ethnic minority groups and individuals from LGBTQ+ communities–into research studies and clinical trials. About 25 research staff completed a set of online courses in the spring of 2023. At the start of the program, only 25% rated themselves as moderately familiar with strategies that may contribute to the successful recruitment of older, underrepresented persons into research studies; the other 75% rated themselves as somewhat familiar, slightly familiar, or not at all familiar. By the end of the 2-month training program, we saw a notable shift: 30% rated themselves as extremely familiar and 70% as moderately familiar with relevant strategies. We hope to hold this training again soon. Also related to this topic, I worked with colleagues in Medicine, Nursing, and Public Health to write a book chapter on the social determinants of physical frailty that highlights the numerous societal-level factors that contribute to health declines among older persons.
Brian: I think this is a hugely important topic. Older adults and persons from minoritized populations are disproportionately affected by the burden of diseases and health problems, but these groups have been historically and vastly under-represented in research studies. This disconnect can mean that the strategies and treatments developed through research to improve health may not be meet the critical needs of those who are most vulnerable. So, we aimed to equip frontline research staff and research managers at Hopkins with knowledge on optimal strategies for the recruitment of diverse older adults into research, with the big-picture goal to improve enrollment of underrepresented older participants–including individuals from racial/ethnic minority groups and individuals from LGBTQ+ communities–into research studies and clinical trials. About 25 research staff completed a set of online courses in the spring of 2023. At the start of the program, only 25% rated themselves as moderately familiar with strategies that may contribute to the successful recruitment of older, underrepresented persons into research studies; the other 75% rated themselves as somewhat familiar, slightly familiar, or not at all familiar. By the end of the 2-month training program, we saw a notable shift: 30% rated themselves as extremely familiar and 70% as moderately familiar with relevant strategies. We hope to hold this training again soon. Also related to this topic, I worked with colleagues in Medicine, Nursing, and Public Health to write a book chapter on the social determinants of physical frailty that highlights the numerous societal-level factors that contribute to health declines among older persons.

