Part One of a two part series on the important role of accelerometry in aging science. The Accelerometry Resource Core (ARC) at COAH has been created to help wearable data become one of the pillars of modern medicine and epidemiology by increasing its accessibility to a wide range of health researchers. To learn more about the ARC, visit accelerometry.org or reach out to Dr. Urbanek directly: jurbane2@jhu.edu or at wearables@jhu.edu.
In recent years, small wearable devices that collect various biological signals have experienced rapid growth in popularity in research and consumer use. Among the many types of wearable sensors, accelerometers that measure the movement of individuals throughout the day and over multiple days are likely the most common. Devices like Fitbit, Apple Watch, and research-oriented Actigraphs have been implemented in various large observational studies, clinical trials, and interventions. These devices are small, waterproof, non-invasive and, in their recent iteration, can be worn like a watch without the need for removing for sleep or bathing.
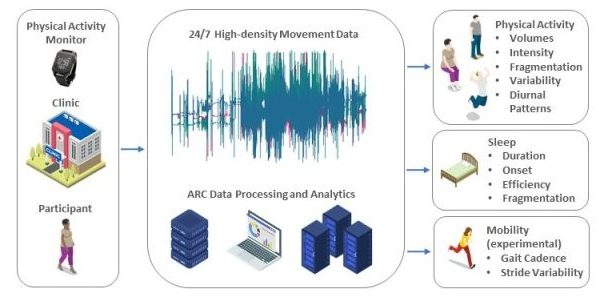
Accelerometers, while most commonly associated with workout tracking and step counting, are capable of much more. Advances in mobile technology over the last decade, have led to smaller sensors with increased memory capacity and battery life, and more affordable prices. As a result, modern, research-grade wearable accelerometers can now collect and store three-dimensional, high-frequency data on human movement continuously over multiple days and nights. For the first time, researchers can gain detailed insight into physical activity, mobility, diurnal rhythms, and sleep characteristics in the context of health.
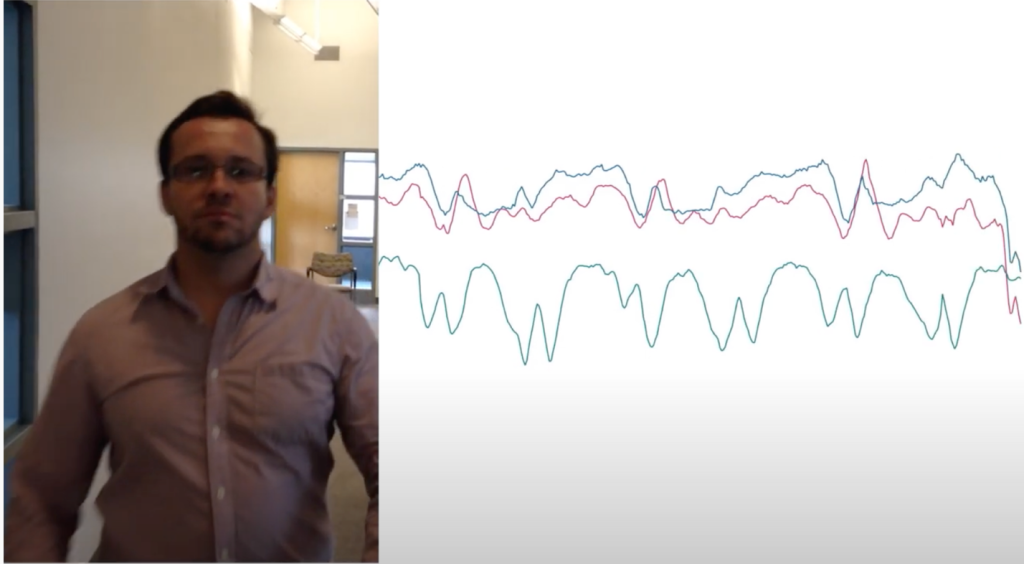
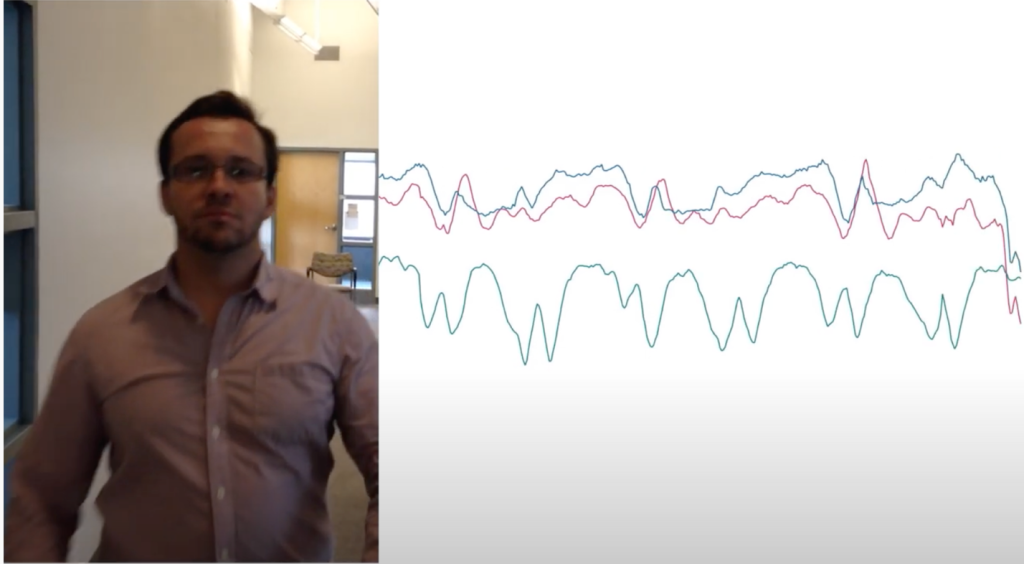
Click here to watch a quick video with Dr. Jacek Urbanek demonstrating just one example of data that a wearable device can pick up from simply clapping his hands, and begin to imagine the bench to bedside possibilities that accelerometry can add to research, clinical trials, and patient centered care.
In the aging population, activities of daily living, mobility, and gait speed are often considered as key measures that can predict various health and quality of life outcomes including functional independence, sensory loss, physical frailty, falls, and death. Advances in wearable technology have not only expanded the ability to effectively monitor and improve the understanding of these measures, but also provide for the remote, multi-day collection of data in free-living conditions that are the most natural to the patient. This results in observations that go beyond the in-clinic snapshot and reflect a more accurate spectrum of movement across a variety of contexts. The importance of the remote collection of clinically relevant data has been further emphasized by the recent COVID-19 pandemic that caused significant limitations to in-person healthcare, especially affecting older, at-risk populations.
Wearable accelerometers were brought into the research spotlight by high-impact, large observational studies focused on general populations. The National Health and Nutrition Examination Survey (NHANES) introduced hip-worn devices in 2003 for the assessment of free-living physical activity and continued this measurement though 2006. Further, NHANES resumed the assessment in 2013 with a new generation of wrist-worn Actigraphs. Similarly, the Study of Latinos (SOL) successfully used wearable accelerometers to monitor longitudinal changes of physical activity across study visits, which is now followed by the assessment with the state-of-the-art devices implemented as a part of Peripheral Artery Disease Study of SOL (PASOS). Internationally, in 2013, the UK Biobank introduced a large-scale cross-sectional collection of wrist-worn accelerometry data to characterize physical activity in the population of the United Kingdom. That success motivated more focused observational studies, clinical trials, and interventions to collect data using wearable devices. In aging research studies, the Baltimore Longitudinal Study of Aging (BLSA) pioneered large-scale monitoring of free-living physical activity and sleep characteristics in older adults, shortly followed by the National Health and Aging Trends Study (NHATS). Overall, the multi-day observation of movements of individuals in real-world settings has been found useful in all areas of health research where physical activity, mobility, or sleep may play an important role. In addition to aging, these areas include frailty, cardiovascular health, recovery after a surgery or clinical stressor, weight loss interventions and obesity, HIV/AIDS, chronic kidney disease, and Alzheimer’s disease, among others.
While wearable devices have been successfully implemented in many existing and new research studies, the technology is still novel and rapidly evolving. The Accelerometry Resource Core (ARC) at the Johns Hopkins Center on Aging and Health has been created to help wearable data become one of the pillars of modern medicine’s clinical practice and research, including epidemiology, by increasing its accessibility to a wide range of health researchers. The ARC offers a full range of collaborative services and provides the expertise, tools, and human resources required for the successful implementation of these measurements. The core is currently collaborating with multiple large-, mid-, and small-size studies by overseeing the collection and providing analytical support for wearable data. Among the most recognizable collaborators are the NHATS, Atherosclerosis Risk in Communities (ARIC), Aging, Cognition and Hearing Evaluation in Elders (ACHIEVE), BLSA, Study To Understand Fall Reduction and Vitamin D in You (STURDY), Characterizing Resiliencies to Physical Stressors in Older Adults (SPRING), PASOS, and Chronic Kidney Disease in Children (CKiD). Throughout these collaborations, members of the ARC have collected, processed, and analyzed cross-sectional and longitudinal data from over 5,000 participants, including over 4,000 older individuals, effectively becoming the largest repository of harmonized, sub-second level, wrist accelerometry data in older adults in the United States.
Stay tuned for Part Two of this article, coming soon!