Dr. Jennifer Schrack is core faculty with the Center on Aging and Health. Among many other outstanding leadership roles, she is the Johns Hopkins University co-PI with the National Health & Aging Trends Study (NHATS). NHATS and the National Study of Caregiving (NSOC) are sponsoring a free 2022-2023 webinar series, which you may learn more about and sign up for here. As a part of this webinar series, Dr. Schrack will deliver a presentation at 12pm ET on November 18th about “Late-life physical activity: Early findings from NHATS’ 2021 accelerometry substudy.” The purpose of this interview is to provide a broad overview of Dr. Schrack’s insightful research and about NHATS.
Tony Teano: Thank you so much for taking the time for this interview. Let’s start by filling in blanks for people who don’t know you. You wear many hats. You’re with several Johns Hopkins centers. You’re a senior leader in the field of aging research and public health. And about a year ago, you were named co-PI of the National Health & Aging Trends Study (NHATS). Tell us more about yourself! What do you do?
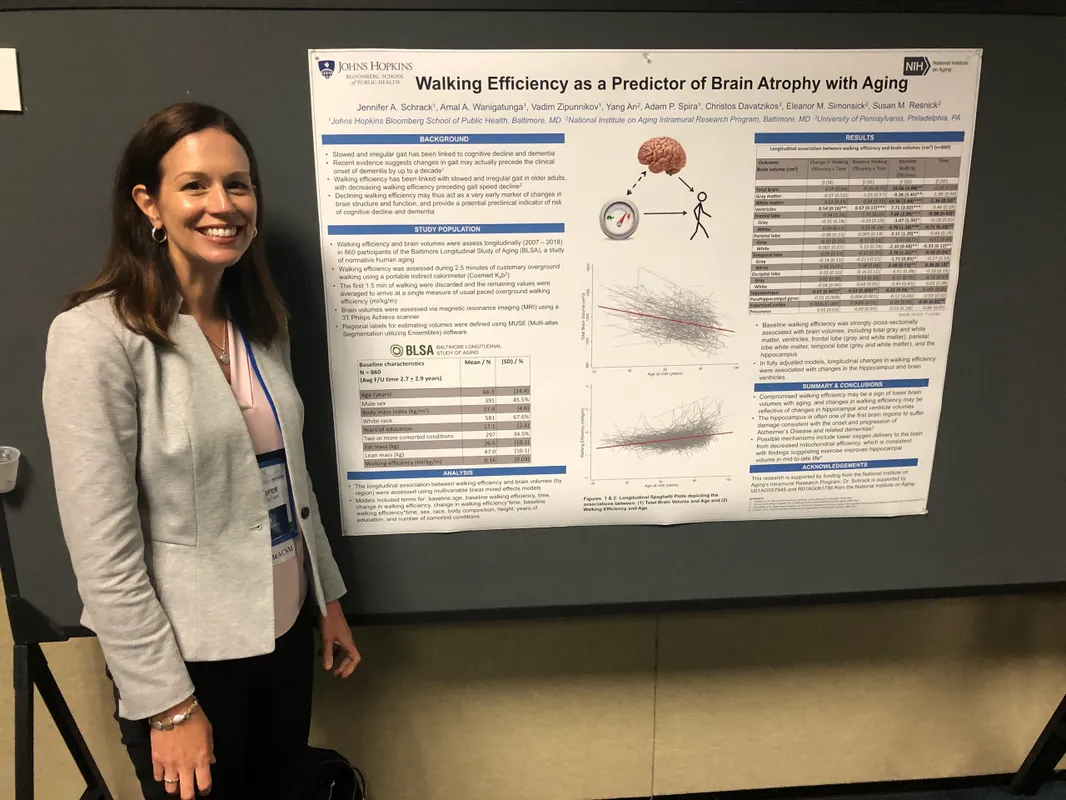
Dr. Schrack: That’s a big question. I am an epidemiologist. I study aging, and I like to say movement and health, and so that encompasses how engaging in movement (or physical activity) can affect people’s health. It is also how changes in movement can be a sign of adverse changes in health. Think about physical activity and mobility as a key piece that I’m interested in. We know physical activity is preventative. We know that it can prevent heart disease and obesity. We think it might be able to prevent cognitive decline, and to preserve mobility and prevent disability with aging. Also changes in the way people move can tell us, perhaps, about subclinical disease and risk of poor outcomes. For example, we think about gait speed as an example that has predicted poor outcomes, disability and death for many years. Now, we’re trying to take that to the next level by having people wear monitors/wearable devices or accelerometers that can help us understand movement in a new dynamic way. We’re looking at a 24-hour movement cycle which can tell us activity, sleep and sedentary time—and all of these things linked together. I study how that influences people’s health, both from a physical side and a cognitive side. And again, how those changes can also help us understand people’s risk of adverse outcomes.
Tony Teano: You have a primary appointment as Associate Professor in the Johns Hopkins Bloomberg School of Public Health in the Division of Epidemiology of Aging, with a joint appointment in the School of Medicine. Maybe it is obvious, but please tell us more about how those appointments enrich and leverage each other?
Dr. Schrack: Actually, it’s a hard question. They complement each other. Epidemiology helps us understand health at the population level. It helps us understand methodological rigor, especially of aging research. But we also have to keep in mind the big questions about why research matters—what does this mean for patients? I think trying to bridge those two schools or those two fields is very, very important—not just for understanding health with aging, but also what are we going to do about it [pertaining to research and translation from bench to bedside application]: What is it? Is it meaningful? Does it matter?
Tony Teano: I appreciate this amazing general overview of your work and your approach to research—and how public health perspectives inform medicine and interventions. Now, let’s turn specifically to NHATS. Please tell us about what NHATS aims to do.
Dr. Schrack: NHATS is a platform for studying late life, disability, and it’s been going on since 2011. Dr. Judy Kasper was the previous Hopkins PI. She unfortunately passed away unexpectedly in August of 2021, and I became a co-PI in September 2021. NHATS is a large panel study of Medicare beneficiaries—people are identified and recruited through their enrollment in Medicare. NHATS strives to be representative of the US population, but we’ve oversampled older adults (those over age 90) as well as older Black adults, and now we’re also over sampling older Hispanic adults, because we realize not enough is known about aging in those populations. NHATS has sampling weights that help us understand the relative contribution of data on people by age, sex, race, ethnicity, and so on, to the study. That’s a way to help make it nationally representative.
Tony Teano: Could you speak more to what types of data NHATS gathers?
Dr. Schrack: We have physical function measures. We have a cognitive battery. We have an extensive health interview—and that interview includes things like understanding people’s ability to do things by themselves in their own home, or whether they need care or assistance, and it also goes a step beyond that by trying to understand accommodations. For instance, someone might not be able to bathe on their own. But if they have a shower chair, then they can. Or they might not be able to walk independently. But if they have a cane, then they can. Understanding accommodations and how they address people’s ability to be independent is valuable information. Also, there’s a link with NHATS and the National Study of Caregiving. If people have a caregiver, we do what we can to interview the caregiver to understand things like caregiver stress, to what extent caregiving is needed, and the types of care provided. All of those things are really important to understanding people’s ability to stay in their homes. Also, we sample people who are in facilities—nursing homes, assisted living, etc.—and we interview them. We also interview the facility to try to understand the kind of services they offer and their associated costs. For researchers, one of NHATS’ most exciting things available with enhanced data is the ability to link all of our research to the data that we collect with Medicare claims. In other words, you can incorporate the cost of certain health conditions, of disability, of cognitive challenges, of Alzheimer’s disease, etc., and connect data from filed Medicare claims into your research. NHATS is an amazing study with a vast amount of data, and it’s a great resource because it is publicly available. Most of this data is freely available on our website. Some of the more sensitive data you have to apply for, but that’s fairly easy to do.
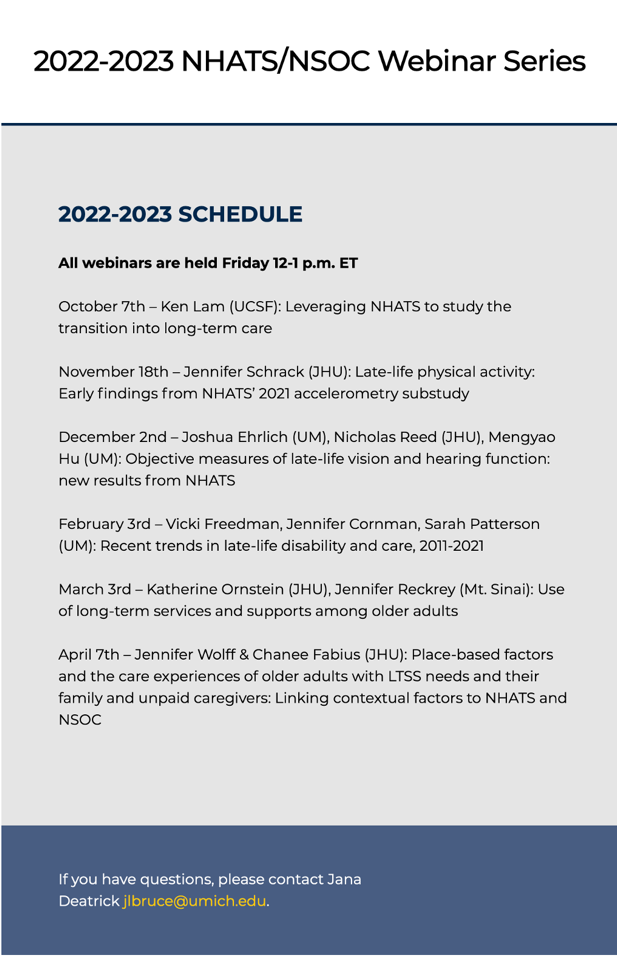
Tony Teano: I noticed a lot of useful and informative information on NHATS’ website—ranging from a new online course for researchers beginning to use NHATS, tutorials, and even a link to 1940 Census data. In particular, I noticed NHATS/NSOC is offering a free speaker series on rich topics such as late-life disability, older adults’ caregiving needs, and new findings in hearing and vision measurements. Please tell us more about these webinars, and what you will talk about as part of it.
Dr. Schrack: The speaker series was actually thought up by my co-PI, Dr. Vicki Freedman with the University of Michigan, as a way to just draw attention to some of the newer and more exciting research that’s being done in NHATS. We’ve reached out to people who we know are doing great work in NHATS, such as Johns Hopkins University colleagues Drs. Jennifer Wolff, Chanee Fabius, Nicholas Reed, and Katherine Ornstein—all of whom will be presenting at this webinar series—and more amazing researchers using NHATS data.
 On November 18th, I will be talking about the introduction of accelerometry to NHATS. This is something we’ve been working on a long time, and it involves a subset of NHATS participants. The study typically runs somewhere around 5,000 to 10,000 older adults. It’s a little bit lower right now, because we need to replenish; we put that off because of COVID-19. In 2021, we selected a substantial number of participants to wear an accelerometer—about 1,000 people—and we got complete and strong data on about 750. The data are really interesting. Because we go to people’s homes, we access a portion of the population not typically seen in research studies. It’s not your typical study where people come into the clinic, we collect data, and they go home. This is where we’re seeing less active, less healthy people. We get people that wouldn’t normally volunteer to be in a research study. And it is exciting because not a lot of information is known about physical activity and movement in these people. Looking at the data so far, we can already see they seem to be less active than people in other studies and other clinical studies. It also picks up where the National Health and Nutrition Examination Survey (NHANES) leaves off; NHANES is a national cross-sectional health and nutrition examination survey. NHANES doesn’t really have a lot of data on people over the age of 80. We have a lot of people in that age range, and we’re going to follow them longitudinally—which hasn’t been done—to understand decline. We’re so excited about the data, and we’re hoping to expand it going forward.
On November 18th, I will be talking about the introduction of accelerometry to NHATS. This is something we’ve been working on a long time, and it involves a subset of NHATS participants. The study typically runs somewhere around 5,000 to 10,000 older adults. It’s a little bit lower right now, because we need to replenish; we put that off because of COVID-19. In 2021, we selected a substantial number of participants to wear an accelerometer—about 1,000 people—and we got complete and strong data on about 750. The data are really interesting. Because we go to people’s homes, we access a portion of the population not typically seen in research studies. It’s not your typical study where people come into the clinic, we collect data, and they go home. This is where we’re seeing less active, less healthy people. We get people that wouldn’t normally volunteer to be in a research study. And it is exciting because not a lot of information is known about physical activity and movement in these people. Looking at the data so far, we can already see they seem to be less active than people in other studies and other clinical studies. It also picks up where the National Health and Nutrition Examination Survey (NHANES) leaves off; NHANES is a national cross-sectional health and nutrition examination survey. NHANES doesn’t really have a lot of data on people over the age of 80. We have a lot of people in that age range, and we’re going to follow them longitudinally—which hasn’t been done—to understand decline. We’re so excited about the data, and we’re hoping to expand it going forward.
Tony Teano: It sounds like a great topic for another blog in the future! For now, I sincerely thank you for your generosity of time for this interview. Your work is fabulous, and I look forward to your NHATS/NSOC presentation on November 18th, and to attending more in the series!
For more information about Dr. Schrack’s research lab team, please visit:
By Anthony L. Teano, MLA
Communications Specialist