Dr. Melissa deCardi Hladek is an Assistant Professor with the Johns Hopkins University School of Nursing, and she is well-known as a researcher-clinician with work focusing on how stress, self-efficacy resilience, and sociocultural factors influence the biology of aging, chronic disease, and frailty. Her research goals are to further understand the role of stress, coping and social determinants of health in aging and develop novel strengths-based, person-environment strategies and policies to mitigate these effects and center the patient’s voice in modern healthcare. Dr. Hladek is a regular participant and collaborator among several COAH workgroups, including the Frailty Working Group, and a Research Education Core grant awardee from the Johns Hopkins Older Americans Independence Center. As an FNP, Dr. Hladek has worked with vulnerable populations experiencing homelessness and incarceration in both rural and urban settings with primarily Spanish-speaking communities. She is the president-elect for the National Association of Hispanic Nurses (NAHN)-DC Metro Chapter and advisor for the Latinx Health Advisory Group at Johns Hopkins School of Nursing.
Earlier this year, she presented a poster at NAHN’s annual conference on “Amplifying the Voice of Older Latinos through Priority Setting,” which serves as the basis of her blog that follows, and which we are delighted to share with you during National Hispanic American Heritage Month 2022. Many thanks to Dr. Hladek for sharing the wisdom of her research on this topic with us now.
 This blog post really comes out of my and my colleagues’ deep desire to meet the healthcare needs of older Latinos in our communities. Latinos currently represent 19% of the total US population, and the number of adults over the age of 65 identifying as Hispanic is projected to double over the next decade. Older Latinos have the highest percentage of any racial or ethnic group living below the poverty line (19.5%), with more than 40% having not completed high school. These socio-economic disparities exacerbate the existing high chronic disease burden and disability experienced by older Latino adults. Multiple studies have identified barriers around language, culture, and healthcare literacy contributing to these poorer health outcomes. Currently, 5.8% of all physicians and 8.4% of all nurses identify as Hispanic or Latino, which puts a disproportionate burden on these providers to deliver culturally concordant care.
This blog post really comes out of my and my colleagues’ deep desire to meet the healthcare needs of older Latinos in our communities. Latinos currently represent 19% of the total US population, and the number of adults over the age of 65 identifying as Hispanic is projected to double over the next decade. Older Latinos have the highest percentage of any racial or ethnic group living below the poverty line (19.5%), with more than 40% having not completed high school. These socio-economic disparities exacerbate the existing high chronic disease burden and disability experienced by older Latino adults. Multiple studies have identified barriers around language, culture, and healthcare literacy contributing to these poorer health outcomes. Currently, 5.8% of all physicians and 8.4% of all nurses identify as Hispanic or Latino, which puts a disproportionate burden on these providers to deliver culturally concordant care.
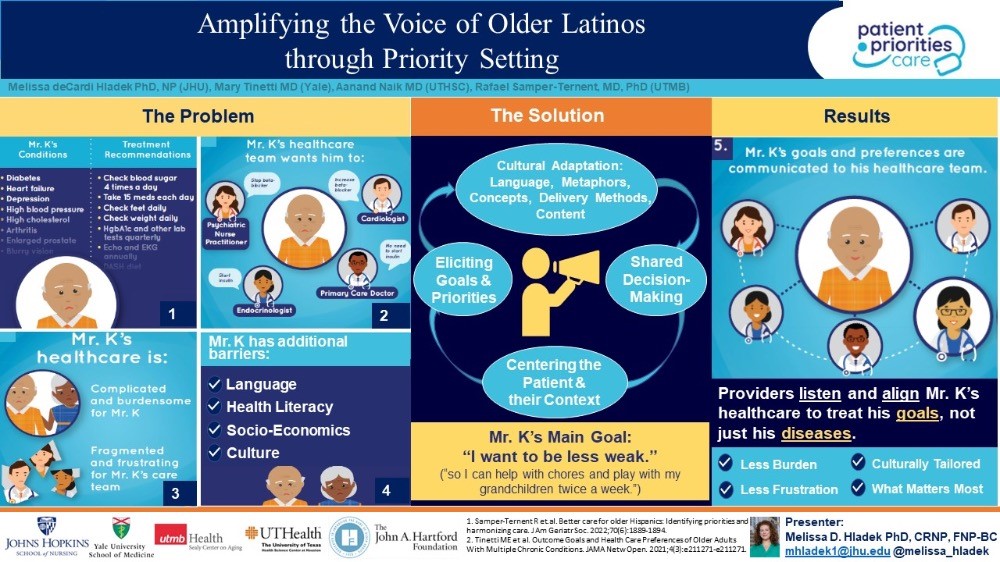
There is an urgent need to develop care pathways for older Latino adults with multimorbidity that centers their experience, and that values in a systematic way and aligns care plans with their priorities. When I think of solutions for these very complicated factors, one evidenced-based approach that immediately comes to mind is entitled “Patient Priorities Care” (PPC). Providing care for older adults with multiple chronic conditions (MCCs) is challenging because of uncertainty of treatment benefits, burden of managing multiple conditions, and inapplicable or conflicting disease-specific guidelines traditionally used to make care decisions. These individuals receive care that is often burdensome, fragmented, and not focused on what matters most to them. In this complicated landscape, shared decision-making, accounting for patient preferences, is the preferred method of decision-making.1,2 Whereas many guidelines focus on disease specific outcomes, older adults often prioritize maintaining independence and quality of life.3 Consequently, obtaining patient preferences facilitates fundamental healthcare system shifts toward “value-based healthcare.”4
As a result of this growing problem in the primary care management of older adults with MCCs, the John A. Hartford Foundation (JAHF) and the Patient Centered Outcomes Research Institute elicited perspectives on how to address these problems from over 150 individuals and dozens of organizations representing patients, family caregivers, health systems, payers, clinicians, and experts in practice change and information technology.1 The consensus solution was entitled “Patient Priorities Care,” a continuous process that begins when patients identify their health priorities. These priorities are used in decision-making among patients and clinicians, centering the patient and their values in the care alignment decision-making process. The work informs the “What Matters” of JAHF’s Age-Friendly Health Systems and, the patient goals-based metrics emanating from JAHF’s Person-Reported Outcome Measures initiative supports uptake of PPC as well. PPC was shown to reduce treatment burden and other metrics related to improved health outcomes in a non-randomized clinical trial (N=366) of older adults with multi-morbidity.5,6 Additionally, we conceptualize centering the patient’s preferences as an integral step in acting upon social determinants of health data and other health equity priorities for older adults, which circles us back to the Latino community.7
PPC was not initially designed with the unique needs of older Latinos in mind. We propose that using an ecological validity model that incorporates an understanding of the whole person, including their lived environment, to culturally tailor PPC will greatly benefit this community. There are eight dimensions of the Ecological Validity Model that could help inform a PPC adaptation including: language; persona (circumstances that commonly affect Latinos); metaphors; content; concepts; goals; methods; and context. Based on my and my colleagues’ lived experience and work within this community, we also acknowledge the heterogeneity of the Latino community and both the religious and cultural belief systems—like “familismo” and “personalismo”—in order to understand healthcare priorities among older Latino adults. In other words, “person-centered” can have a more expanded meaning to include family members or caregivers in the Latino context.
It is of critical importance to account for the unique strengths and health disparities attributed to existing social determinants of health when adapting interventions, like PPC, to the older Latino adult population. A PPC adaptation for the Latino population holds promise to amplify the patient’s voice, improve health outcomes and promote health equity.
References:
- Cooper Z, Courtwright A, Karlage A, Gawande A, Block S. Pitfalls in communication that lead to nonbeneficial emergency surgery in elderly patients with serious illness: Description of the problem and elements of a solution. Ann Surg. 2014;260(6):949-957. doi:10.1097/SLA.0000000000000721
- Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140(1):54-59. doi:10.7326/0003-4819-140-1-200401060-00012
- Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061-1066. doi:10.1056/NEJMSA012528
- Mooijaart SP, Carpenter CR, Conroy SP. Geriatric emergency medicine-a model for frailty friendly healthcare. Age Ageing. 2022;51(3). doi:10.1093/AGEING/AFAB280
- Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient Priority-Directed Decision Making and Care for Older Adults with Multiple Chronic Conditions. Clin Geriatr Med. 2016;32(2):261-275. doi:10.1016/J.CGER.2016.01.012
- Tinetti ME, Naik AD, Dindo L, Costello DM, Esterson J, Geda M, et al. Association of Patient Priorities–Aligned Decision-Making With Patient Outcomes and Ambulatory Health Care Burden Among Older Adults With Multiple Chronic Conditions: A Nonrandomized Clinical Trial. JAMA Intern Med. 2019;179(12):1688-1697. doi:10.1001/JAMAINTERNMED.2019.4235
- Samper-Ternent R, Tinetti M, Jennings LA, Wong R, Arney J, Naik AD. Better care for older Hispanics: Identifying priorities and harmonizing care. J Am Geriatr Soc. 2022;70(6):1889-1894. doi:10.1111/JGS.17748
By Melissa deCardi Hladek, PhD, MSN, RN, CRNP, FNP-BC

